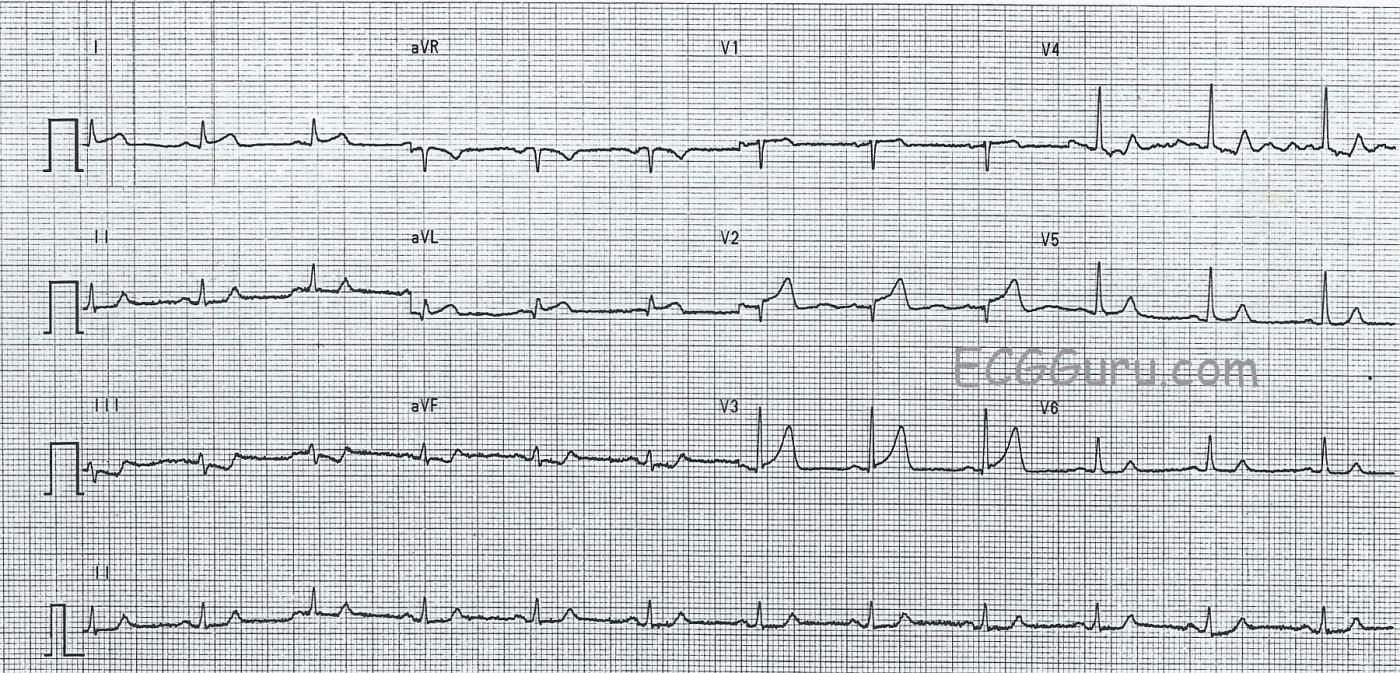
This ECG is from a 65-year-old woman who presented to the Emergency Department with a complaint of chest pain. We have no other clinical information.
There are several subtle, but real, abnormalities on the ECG that should be evaluated in conjuction with her clinical situation. This is a good ECG to discuss with your more advanced students who have mastered recognition of blatant ST elevation M.I. (STEMI). But, let’s start with what is NORMAL here.
NORMAL FEATURES The normal findings are: normal sinus rhythm at about 68 bpm. The rhythm is regular without ectopy. The intervals are within normal limits. The frontal plane axis is normal. The T waves are all upright.
ABNORMAL FEATURES There is subtle ST segment elevation in Leads V1 through V3, and in I and aVL. The shape of the ST segments is concave upward, or normal. In a young, asymptomatic patient, we probably would not be at all concerned about this amount of ST elevation. However, this is an older patient with chest pain. In the chest leads, the R wave progression is interrupted, as the QRS goes abruptly from negative to positive in Lead V3. This could be due to loss of r waves ( pathological Q waves forming) in V1 and V2 lead placement, or something else.
In addition, the inferior leads (II, III, and aVF) show ST flattening, with ST depression in Lead III. Probably the best way to approach such subtle changes in a symptomatic patient is to repeat the ECG frequently while initiating evaluation and treatment of the chest pain. Often, ST segments will change rapidly during an ischemic episode. Lead aVL appears to have a pathological Q wave, but that lead sometimes has a septal q wave, which is normal. Having a prior ECG for comparison is also very helpful for differentiating acute changes.
TEACHING OPPORTUNITIES This tracing can help you teach students that not all cardiac patients will present with flagrant STEMIs, and we much learn to see subtle abnormalities and consider them in light of clinical features – history, symptoms, labs, and ECG changes.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Making the Most Out of What We Have — 1st Diagonal Occlusion
Interesting tracing for the reasons Dawn mentions. Unfortunately, all we know is that the patient is a 65-year old woman who presented to the ED with new chest pain. That said, the KEY to this tracing lies in the limb leads. The precordial leads are problematic because: i) ST elevation is limited primarily to lead V2, with lesser ST elevation in V3 and minimal (but present) ST elevation in lead V1; ii) ST segment shape in the chest leads is concave-up (ie, “smiley”-configuration), which resembles that often seen in repolarization variants; and iii) R wave progression is unexpectedly abrupt as Dawn mentions — which to me suggests a problem with lead placement. But that leaves me not knowing what is really going on in the chest leads — UNTIL I look at the limb leads.
First — there is low voltage in the limb leads. This low voltage does not prevent interpretation, but it does make such interpretation more challenging.
Note the small q wave and ST elevation in lead aVL. By itself, this might not be “telling” — but it is when you consider that: i) the ST segment in lead I is also slightly elevated (subtle-but-real); ii) there is “mirror-image” ST-T wave depression not only in lead III, but also in lead aVF; iii) lead II though subtle clearly shows ST straightening and slight depression with an abnormally peaked terminal T wave (that DOES support my theory of reciprocal ST-T wave changes in each of the inferior leads); and iv) we DO have some ST elevation in the chest leads.
BOTTOM LINE: In a 65-year old woman with new chest pain, this ECG to me is highly suggestive of new ongoing acute STEMI. The finding of ST elevation in lead aVL with reciprocal inferior ST depression and ST elevation in the chest leads that is primarily limited to lead V2 suggests that the “culprit artery” is likely to be proximal in the LAD (Left Anterior Descending) artery system, and likely the 1st Diagonal branch.
Of course, if it turns out that precordial lead placement is indeed off, and that leads V3,V4 really do look more like lead V2 — then rather than the 1st Diagonal branch, the “culprit artery” could be the proximal LAD itself. Regardless, we see enough indicate prompt cath for diagnosis and hopefully acute reperfusion therapy.
Ken Grauer, MD www.kg-ekgpress.com [email protected]