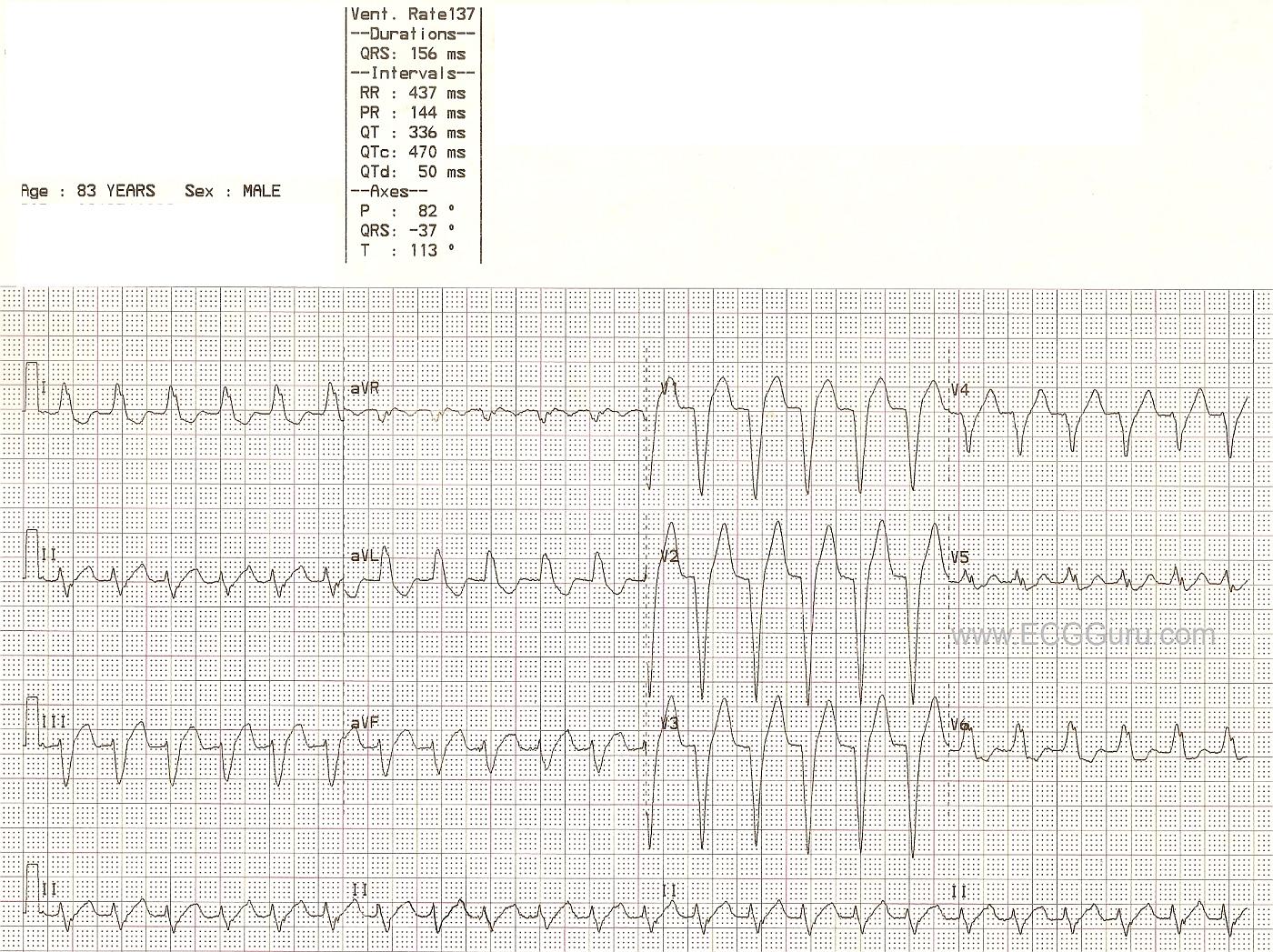
This ECG shows a wide-complex tachycardia with a rate of 137/minute. No patient information is available other than what is on the ECG. Here, we will comment for the BASIC LEVEL learner, and allow the ECG Gurus out there to add INTERMEDIATE and ADVANCED level comments.
Beginners and emergency workers should ALWAYS be cautioned to treat all wide-complex tachycardias as VENTRICULAR TACHYCARDIA until proven to be something else. V Tach is a life-threatening dysrhythmia, and there should be no delay in treatment. That being said, not all WCTs are V Tach. The most common "mimic" of V Tach is left bundle branch block. LBBB can appear along with any supraventricular rhythm, including sinus rhythms, atrial tachycardias, atrial fibrillation, and junctional rhythms. The diagnostic criteria for LBBB are: wide QRS (.12 seconds or more), supraventricular rhythm, negative QRS in V1 and positive QRS in V6 and Lead I. This ECG meets the criteria for LBBB, except that the supraventricular rhythm is hard to prove. On one hand, P waves are not seen - or at least not easily. On the other hand, the ECG machine has recorded a PR interval and a P wave axis. What do you think?
Some of the criteria that would favor the diagnosis of V Tach are not present here: precordial concordance (all QRS complexes in V1 through V6 pointing in same direction), V6 with a negative QRS, AV dissociation. An extreme axis, especially extreme right, would favor V Tach. This ECG has an abnormal left axis, which is possible in V Tach AND in LBBB. For a more thorough discussion by ECG Guru Jason Roediger of the criteria for differentiating V Tach from LBBB and other aberrancy, go to this LINK.
In an emergency setting, WTCs are most often V Tach. However, should the rhythm turn out to be SVT with aberrant conduction, the usual V Tach treatment protocols would do no harm. For instance, if the patient is deemed to be "unstable", electric cardioversion is recommended for both V Tach and SVT. If the patient is stable, the emergency drugs usually recommended are generally safe for both rhythms.
Care should be taken to differentiate SINUS tachycardia from SVT or V Tach. Sinus tachycardia usually has an obvious physiologic cause (hypoxia, hypovolemia, fear, pain, fever, etc.). Sinus tachycardia also will be variable in rate, slowing as the cause is alleviated, or speeding if the problem causing the tachycardia becomes worse. It may require a long period of observation to determine that the rate is gradually slowing or speeding up. One would hope to find P waves at some point in sinus tachycardia, and a 12-lead ECG is a great help.
WE LOOK FORWARD TO COMMENTS FROM OUR MEMBERS.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
A Regular WCT that May Be Supraventricular
I agree with general assessment by Dawn of this interesting tracing.
We see an almost precisely regular WCT (Wide-Complex Tachycardia) at a rate of ~140/minute. I say "almost precisely regular" - because I believe there are some very small irregularities in this tracing. I say this after measuring multiple times .... (something I'd never have the luxury of doing if this patient was in front of me! ). I don't think the tiny irregularity I detect is enough to call this AFib - and both AFlutter and VT may have some irregularity - so this is really not helpful to our differential diagnosis.
So we are left with a regular (at least almost regular) WCT rhythm without evidence of sinus P waves. Since we don't know the history or clinical condition of this patient - we have to speculate:
I've written up a similar case with step-by-step description on my ACLS Comments #11. GO TO: https://www.kg-ekgpress.com/acls_comments-_issue_11/ - The most important points to make about this tracing (assuming the patient remains hemodynamically stable) are the following:
BOTtOM LINE: You do NOT have to be certain of the rhythm diagnosis at the time you initiate treatment. This is one such case in which I don't think there is any way to be certain before beginning treatment. As long as you remain ready to cardiovert at the first sign of patient deterioration - it is perfectly appropriate to proceed with Adenosine as an initial drug given as a diagnostic/therapeutic trial.
P.S. This might be a time to try an additional monitoring lead such as a Lewis Lead. This rhythm could be AFlutter - and use of a Lewis Lead might demonstrate flutter or other atrial activity.
Ken Grauer, MD www.kg-ekgpress.com [email protected]