These two ECGs are from a 77-year-old woman who was complaining of palpitations and mild shortness of breath. She stated a history of atrial fibrillation. She was alert, with a systolic BP over 120. At the hospital, she was found to have cardiomyopathy, resulting in global hypokinesis. She also had significant coronary artery narrowing in her left main, left anterior descending, and circumflex, which were treated with coronary artery bypass graft surgery.
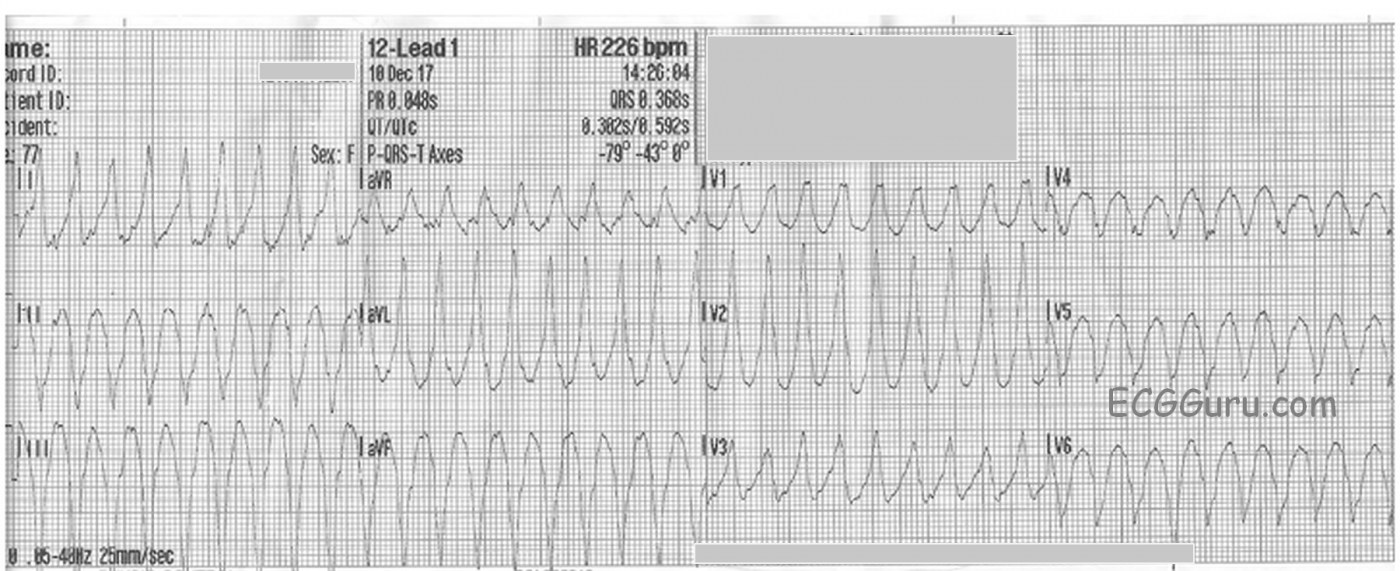
The first ECG was taken on arrival of the EMS crew at the patient’s home. It shows ventricular tachycardia, rate 226 bpm, All WCTs should be considered to be ventricular tachycardia until proven otherwise. While WCT can sometimes be difficult to definitively diagnose in the field, this ECG has many features which favor the diagnosis of VT, including:
· An extremely wide QRS (I measure .24 sec., the machine measures .368 sec.).
· An extreme left axis deviation (aVF is all negative).
· Absence of either RBBB or LBBB pattern, with a completely negative QRS in V6. This all negative V6 places the liklihood of the rhythm being VT to about 100%.
· No obvious P waves (although the machine gives a P wave axis and a PR interval).
· No RS complexes seen in the precordial leads (V1-V6).
·
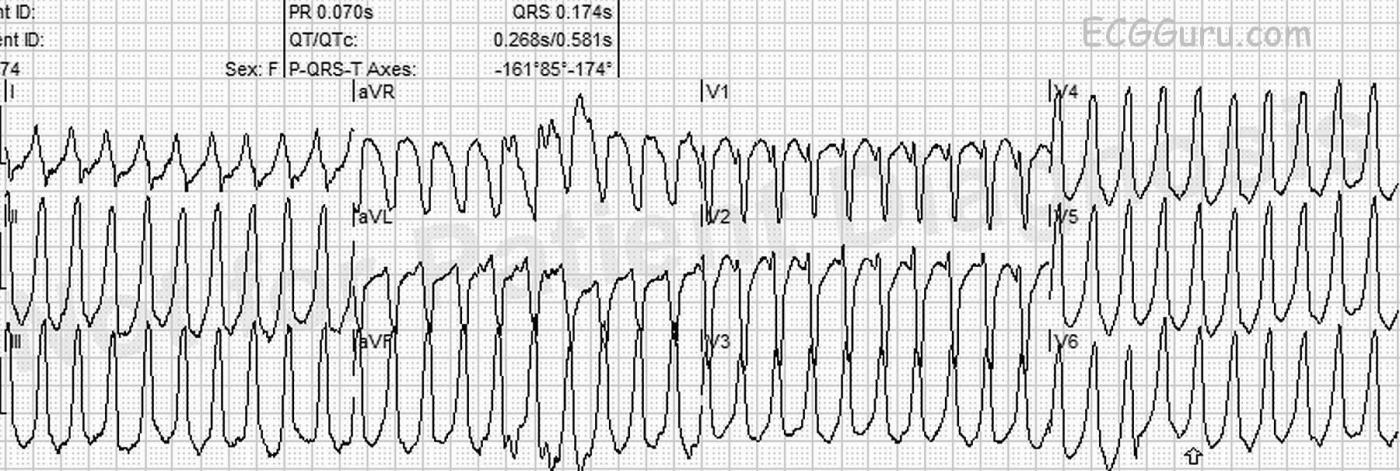
The second ECG was taken three minutes later, with no change in the patient’s symptoms. (The age is different because a different crew took the tracing, but it was confirmed to be from the same patient.) The heart rate is now 239 bpm, and she still has a wide-complex tachycardia. The morphology of the QRS complexes has changed. This now has the pattern of right ventricular outflow tract ventricular tachycardia (RVOT). RVOT originates from the area around the outflow tract of the RV, or from the tricuspid annulus.
Characteristics of RVOT include:
· Heart rate > 100 bpm
· Atrioventricular dissociation
· QRS width > .12 seconds.
· Left bundle branch block morphology
· Inferior / rightward axis (around +90 degrees)
RVOT often responds to adenosine.
RVOT usually occurs in the absence of structural heart disease, or occasionally in the setting of arrhythmogenic right ventricular dysplasia/cardiomyopathy. This patient certainly was found to have serious heart disease, making the diagnosis of idiopathic RVOT unlikely, and adenosine not recommended.
Myopathy as severe as this patient’s frequently causes ventricular ectopy and ventricular tachycardia, which can add to the severe cardiac output issues the patient faces.
References: http://ecg-interpretation.blogspot.com/2012/01/ecg-interpretation-review-35-sct-vt.html/ ; https://lifeinthefastlane.com/collections/ ; https://stanfordhealthcare.org/medical-conditions/blood-heart-circulation/ventricular-tachycardia/types/right-ventricular-outflow-tract-tachycardia.html
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.