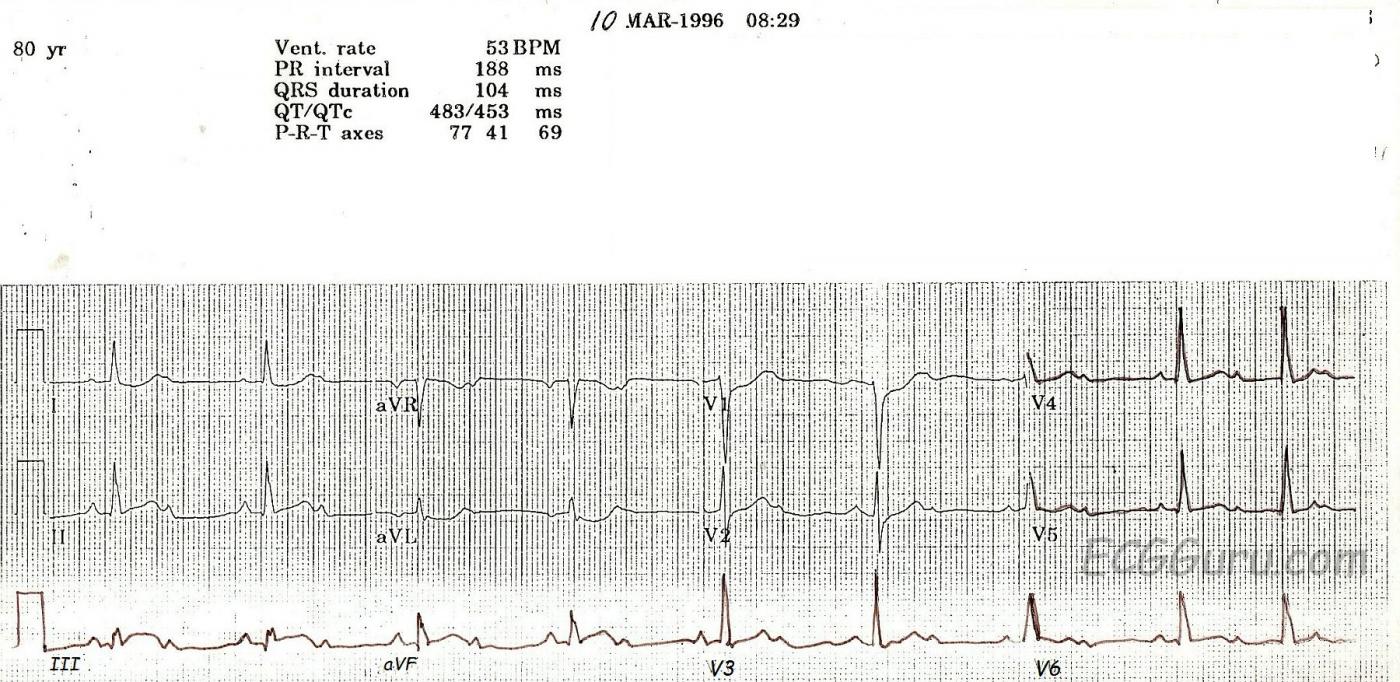
This ECG is from an 80-year-old woman who had an acute inferior wall M.I. with a second-degree AV block.
Some people incorrectly call ALL second-degree AV blocks that are conducting 2:1 "Type II". This is incorrect, as Mobitz Type I can also conduct with a 2:1 ratio. The progressive prolongation of the PR interval will not be seen with a 2:1 conduction ratio, because there are not two PR intervals in a row.
This is a good example of a Type I, or Wenckebach, block which is initially conducting 2:1. At the end of the ECG, two consecutive p waves conduct, showing the "progressively-prolonging PR interval" hallmark of a Type I block. Type I blocks are supraHisian - at the level of the AV node - and generally not life-threatening. Blocks that are conducting 2:1 present a danger, however, in the effect they have on the rate. Whatever the underlying rhythm is, the 2:1 block will cut the rate in half! This patient has an underlying sinus tachycardia at 106, so her block has caused a rate of 53. In light of her acute M.I., that rate is probably preferable to the sinus tach. This patient’s BP remained stable, and she did not require pacing.
The ST signs of acute M.I. are rather subtle here. Note the "coving upward" shape in Lead III, and the reciprocal depressions in I, aVL, V1, and V2. Type I blocks are common in inferior wall M.I., since the AV node and the inferior wall often share a blood supply - the right coronary artery.
While the print quality of this ECG is not the best, it is a great teaching ECG because it starts out with 2:1 conduction, then at the end of the strip, proves itself to be a Wenckebach block.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
A lot to be Learned from this strip!
Another tell-tale sign that this 2:1 block is really a Mobitz I is the narrow QRS complex. A Mobitz II block is really a bifascicular block that is intermittently blocking in the third fascicle creating a momentary third degree block (hence the need for an emergent pacemaker insertion). So a Mobitz II block is virtually always in the presence of a wide QRS complex. Certainly, a Mobitz I block can occur in the presence of a pre-existing bundle branch block, but that doesn't happen very often. On the other hand, a Mobitz II block with a narrow QRS complex would be very unusual indeed.
Although this ECG is an exception, Mobitz I block is very, very frequently accompanied by a baseline first degree AV block.
The other issue relates to the acute inferior infarction. On many occasions, the ST deviation in the inferior leads is very subtle or simply not there. But ST depression in lead aVL is almost diagnostic of inferior wall MI. Certainly, LBBB and LVH can cause ST depression in aVL, but aside from those two entities, the next most common cause would be a reciprocal change during an inferior MI (in the context of a patient with symptoms compatible with ACS). The reciprocal change of ST depression in aVL very often appears well before the STE in the inferior leads.
Another point that I make in my classes is that ischemic ST depression does NOT localize! If a patient is having chest pain and there is ST depression in II, III and aVF, or I and aVL, or V1 - V3 -- that's NOT ischemia. Those are reciprocal changes!
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
Thanks for the GREAT comments, JWJ
Some very important teaching points were made by JWJ above, and of course, we agree completely. For an example of a TYPE II AV block that starts out as a 2:1 AVB, go to this LINK. Thanks again, JWJ.
Dawn Altman, Admin