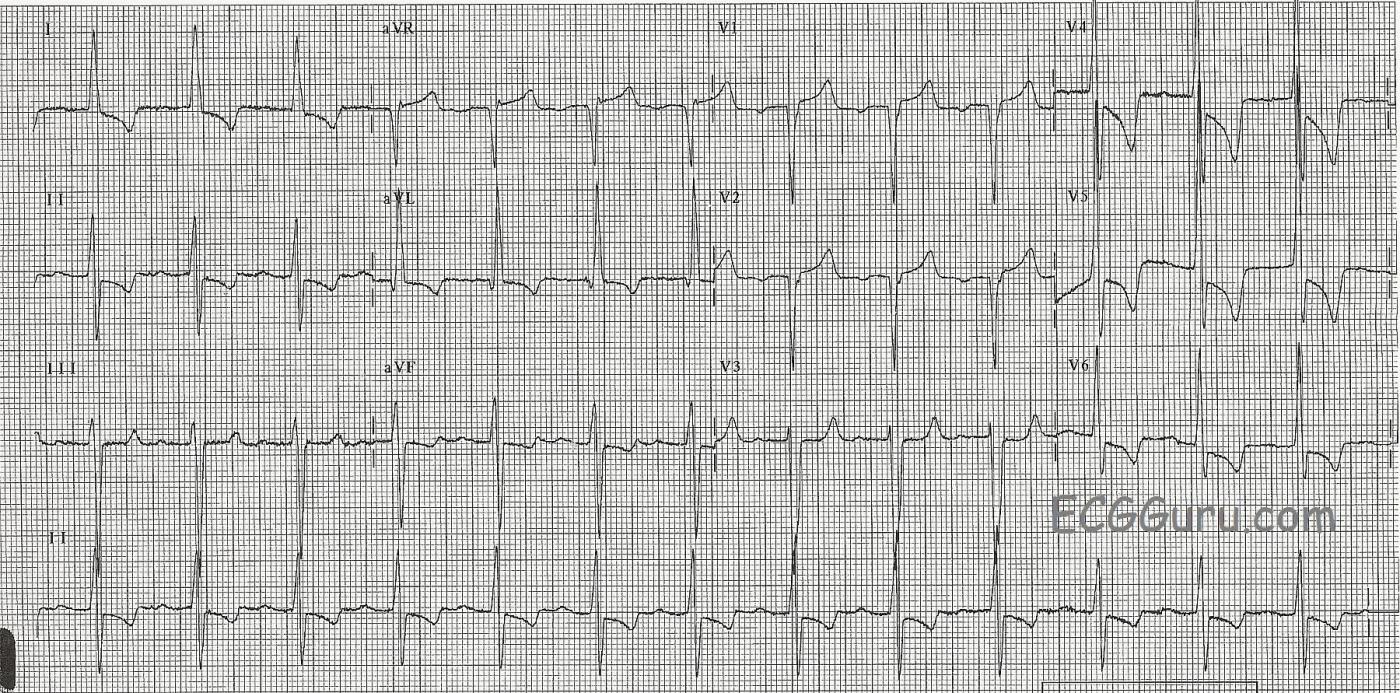
This ECG is from a man with left ventricular hypertrophy. LVH causes taller-than-normal QRS complexes in leads oriented toward the left side of the heart, such as Leads I, II, aVL, V4, V5, and V6. Leads on the opposite side, such as V1, V2, and V3, will have deeper-than-normal S waves. A commonly-used criteria for determination of LVH is the Sokolow-Lyon index: S in V1 + R in V5 or V6 (whichever is larger) ≥ 35 mm (≥ 7 large squares); and R in aVL ≥ 11 mm. There is no perfect ECG criteria for determining LVH. The most accurate way to evaluate the size and thickness of the chambers of the heart is echocardiogram (ultrasound). Frequently, there is left axis deviation, especially if the hypertrophy is confined to the left ventricle.
The left ventricle can be enlarged for many reasons, some worse than others. Athletes naturally enlarge the heart, as they work the muscle. Pathological causes for LVH can include anything that strains the heart as it pushes against increased afterload, such as hypertension and aortic stenosis, and diseases of the myocardium, such as cardiac myopathies.
ECGs that show LVH often have signs of other problems, including enlargement of the atria and/or the right ventricle. LVH does not preclude the diagnosis of acute coronary insufficiency or myocardial infarction, but it can make the signs of other problems more difficult to see. When LVH is caused by a pathological condition, we often see the "strain" pattern, which is ST depression and T wave inversion in leads with upright QRS complexes (the lateral leads). A reciprocal ST elevation can occur in the right-sided leads, which can be confusing to those looking for STEMI.
Dr. Ed Burns, of Life In the Fast Lane, has a very good page describing the criteria and facts of LVH. Dr. Ken Grauer discusses LVH Here, and in all of his publications and on his website.
If you look closely at this ECG, you will find other abnormalities, and clinical corelation is always warranted.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
LVH - when ST-T waves may be MORE than just "Strain"
The Instructor Collection ECG for this week provides an excellent illustration of how it may be difficult with LVH to determine if there is more than just "strain" reflected by ST-T wave appearance. I think there is more than just LVH in this tracing. I'd interpret this ECG as follows:
Ken Grauer, MD www.kg-ekgpress.com [email protected]