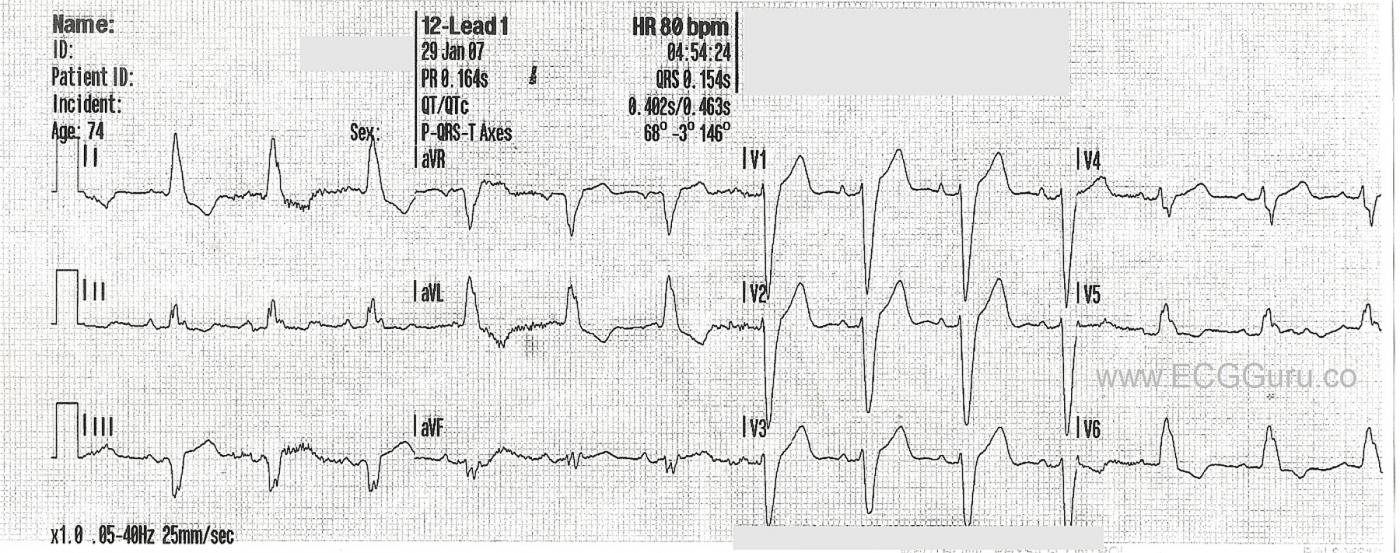
This ECG shows a “classic” left bundle branch block pattern.
The ECG criteria for left bundle branch block are:
· Wide QRS (.12 seconds or greater)
· Supraventricular rhythm (ventricular rhythms do not travel via the LBB)
· The QRS in V1 is negative, and the QRS in Leads I and V6 are positive.
The left bundle branch (LBB) can be blocked permanently, temporarily, intermittently, or in the because of a fast rate. When the LBB is blocked, conduction proceeds from the AV junction down the right bundle branch, depolarizing the right ventricle. The impulse travels from the right ventricle across the left ventricle, cell by cell. Conduction is slower this way, and there is asynchrony of the ventricles. This slow conduction and asynchrony of the two ventricles causes widening of the QRS complex.
NOTE: It is "normal" for wide-complex rhythms to have ST segment elevation in leads with negative QRS complexes and ST depression in leads with positive QRS complexes. This can make it a bit difficult to determine the ST changes of acute M.I.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
LBBB with some Interesting Findings
Ken Grauer, MD www.kg-ekgpress.com [email protected]