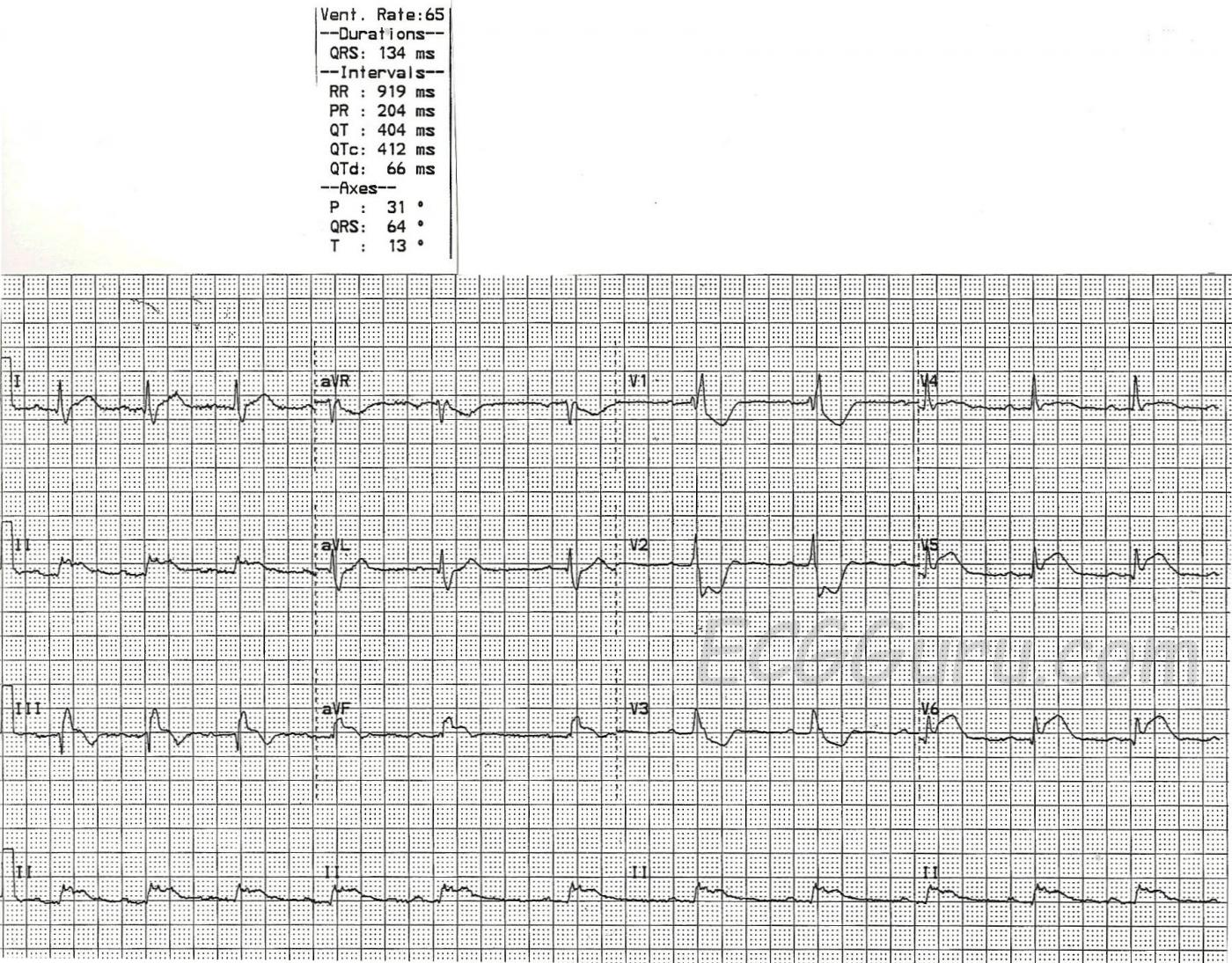
This ECG shows two obvious abnormalities, right bundle branch block AND inferior wall M.I. It is also a good teaching example of how the terminal wave of RBBB can be mistaken for the ST elevation of M.I.
First, check this ECG to see if it meets the criteria for right bundle branch block:
1) The QRS will be wide. That is, it will be greater than or equal to .12 seconds (120 ms). In this case, the QRS is 134 ms.
2) The rhythm will be supraventricular. Supraventricular rhythms originate from above the ventricles. This ECG has P waves before each QRS. Even though the rhythm is irregular, slowing down during this recorded period, it is a sinus rhythm.
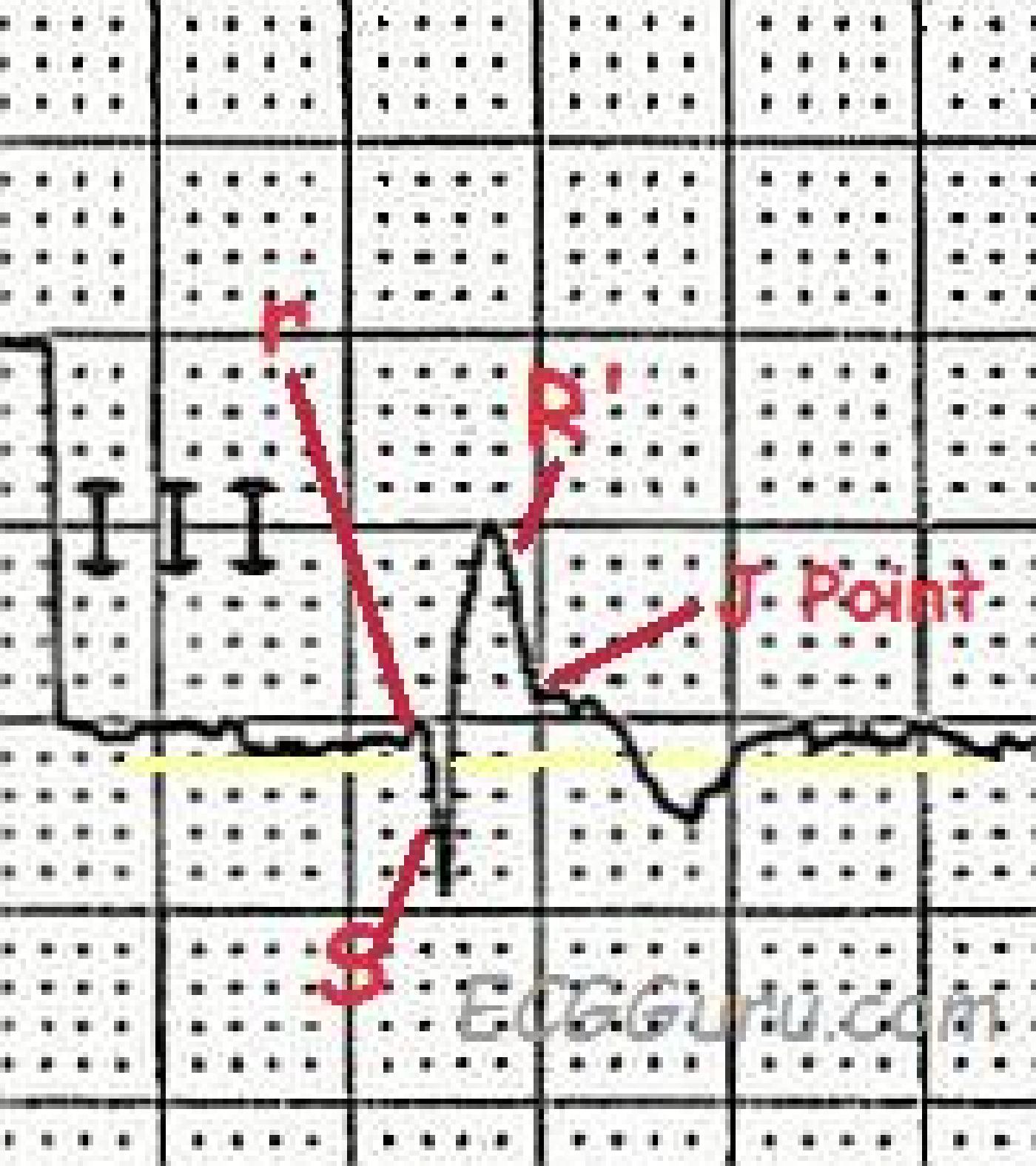
3) The QRS will have a terminal wave after the "normal" part of the QRS. This represents the right ventricle depolarizing late. It is very easily seen in V1, which normally has an rS pattern, and with RBBB has an rSR' pattern, making it appear upright. V6 and Lead I will show this terminal wave as a wide little s wave.
As mentioned, there is also an acute inferior wall M.I. here. The ST segment elevation in Leads II, III, and aVF are actually quite subtle. The flat top of the ST segments gives them away as abnormal, along with the associated ST elevations in V5 and V6, and the reciprocal ST depressions in V1 through V3. Normally, in IWMI, there will be reciprocal ST depressions in Leads I and aVL, but the elevations they are reflecting are very subtle, and so, therefore, are the depressions.
The tricky thing about this ECG is that you must look carefully at the inferior wall leads to see the true ST elevation, which, as mentioned, is subtle. The RBBB terminal wave of the QRS complexes in Leads III and aVF is upright, and is often mistaken for ST elevation. Remember, ST segments are smooth from the end of the QRS to the peak of the T wave. See the detail illustration.
This ECG is suitable for your classes from beginner level (rate variation in sinus rhythm) through advanced (clinical significance of RBBB in acute M.I.). It also offers an example of reciprocal ST changes, and of a situation where the inferior leads II, III, and aVF are related to the low lateral leads V5 and V6 by a shared blood supply.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
LOTS to Discuss- Acute Inf-Post-Lat STEMI, RBBB, LCx Occlusion
Ken Grauer, MD www.kg-ekgpress.com [email protected]