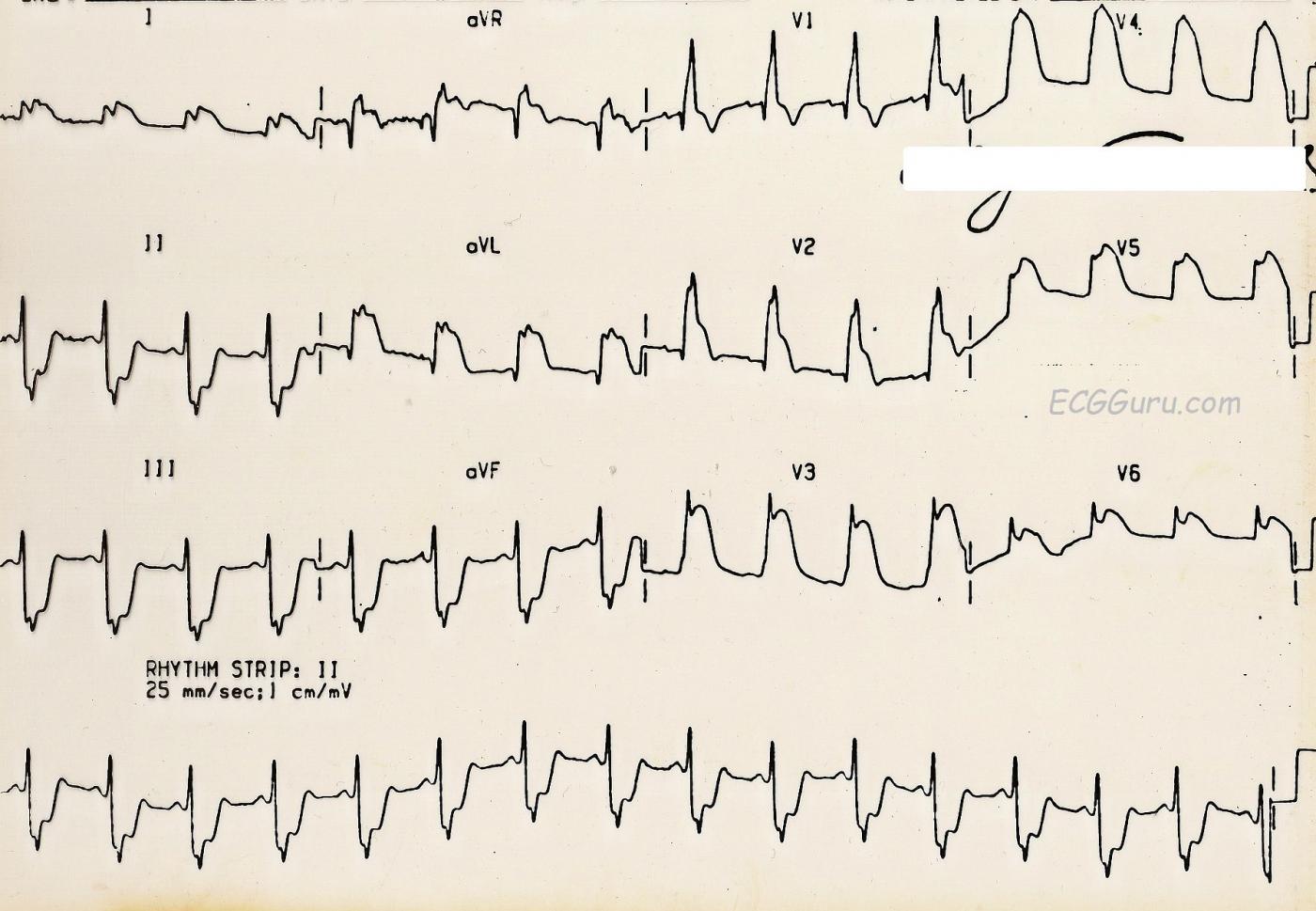
This ECG depicts an extensive and ultimately, fatal, injury. There is marked ST segment elevation in Leads V2 through V6 (anterior wall). There is also ST elevation in Leads I and aVL (high lateral wall). The ST elevation in aVR is indicative of a very proximal lesion in the left coronary artery, which supplies the anterior wall, including the anterior portion of the septum, the high lateral wall, and, in this case, the low lateral wall. The inferior leads, II, III, and aVF, show reciprocal ST depression.
This is an old ECG - the computer readings of the rate and intervals is lost, as is the grid. But the rate here appears to be about 80 bpm and the QRS is widened. There is a right bundle branch block ECG pattern, which is not surprising given the extensive septal damage. Normally, the criteria for RBBB on the ECG includes an rSR' pattern in V1 (seen here) and a small, wide s wave in Leads I and V6. This s wave is not seen here, presumably due to the effects of the ST elevation in those leads.
What matters clinically in a patient like this is not whether there is RBBB or another type of interventricular conduction delay. This patient needs immediate restoration of blood flow through the LCA and intensive medical/nursing care. As mentioned before, this patient did not survive, in spite of being brought to a hospital. We do not know the exact mechanism of death or treatment course in this case.
If you are teaching students to use multiple leads in assessing rhythm, this is a great example of how one or two leads can be very misleading. I have used this ECG's V4 in an excercise illustrating this concept. Shown V4, many people would call this "AIVR" or "V Tach". Seen in context with the other leads, it is obvious that we are looking at ST elevation that is as high as the R wave. Two leads are better than one, and twelve are better than two.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Acute Left Main Occlusion - with RBBB/LAHB
Ken Grauer, MD www.kg-ekgpress.com [email protected]