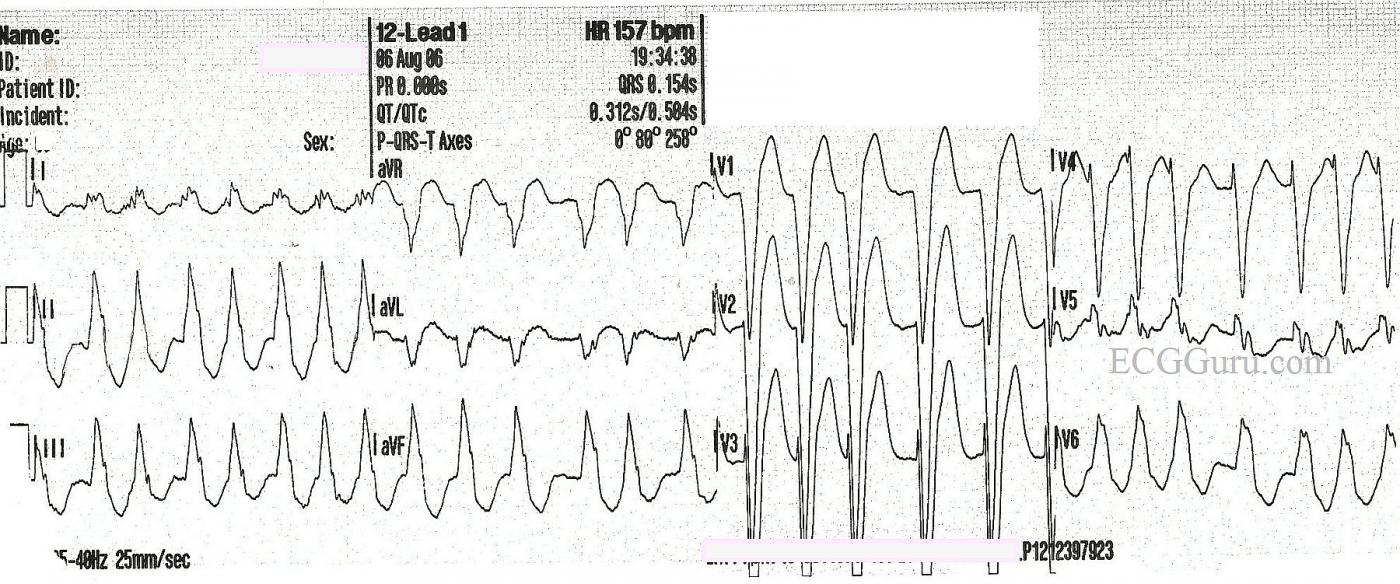
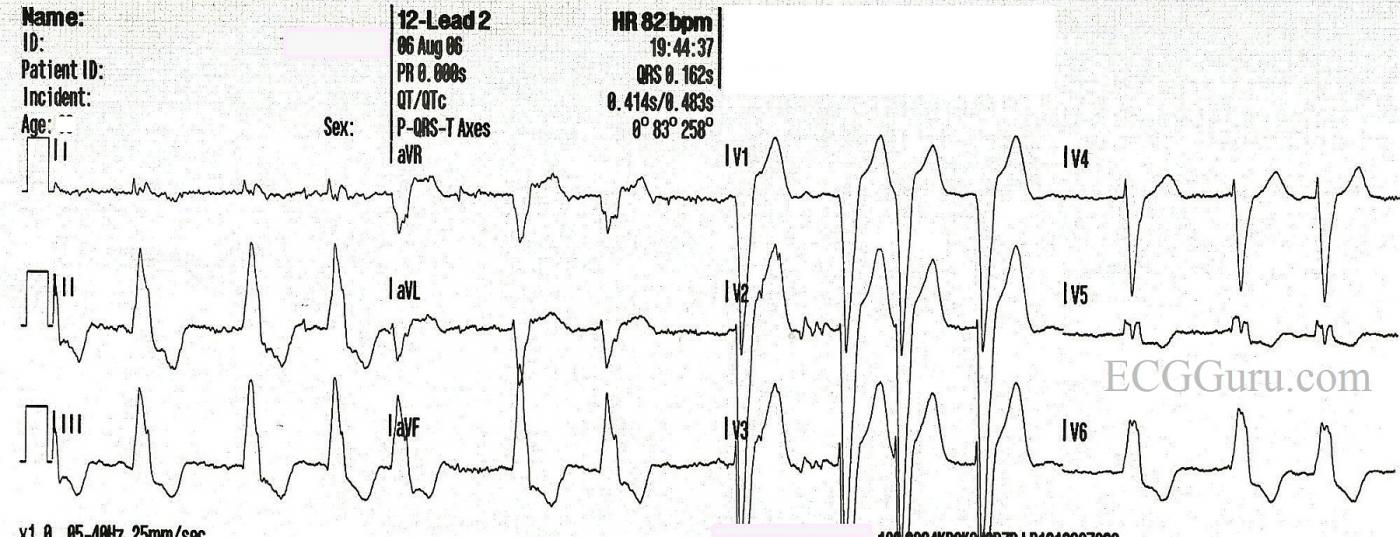
This is a good example of atrial fibrillation with left bundle branch block. You get two ECGs with this one, because the patient presented to EMS with a fast heart rate, and the rate was slowed with the drug diltiazem. We do not have any other patient information, unfortunately.
In the first strip, we see a wide-complex tachycardia. In an emergency situation, with an unstable patient, this rhythm could safely be treated using an emergency ventricular tachycardia (VT) protocol. In fact, all WCTs should be considered to be VT until proven otherwise. In most emergency settings, the unstable VT patient would be electrically cardioverted, which will often convert atrial fibrillation as well. The stable patient with this rhythm would be treated with an antiarrhythmic drug, such as amiodarone. This may convert or slow down atrial fib. So, in the initial stages of treatment, differentiating between VT and A Fib is not the first priority. Assessing the patient's hemodynamic stability and addressing the rate if necessary are the priorities.
So, how do we know this is NOT VT? It can be difficult, but in this case, the rhythm, even though fast, is very irregular. VT is not always perfectly regular, but this irregularly-irregular rhythm points to atrial fibrillation. Also, the pattern of the QRS morphology fits with LBBB. The criteria for LBBB are: 1) supraventricular rhythm, 2) wide QRS, 3) negative QRS in V1 with positive QRS in Leads I and V6. If we assume the rhythm is atrial fibrillation, we meet the first criteria. The other two are self-evident.
After the medication is administered, 10 minutes later, we see the rate slow down. There is no change in the irregularly-irregular rhythm, and the LBBB pattern remains. All that has changed is the rate and, hopefully, the patient's symptoms. This confirms that the original rhythm was not VT.
Remember, atrial fib lowers cardiac output because there is no P wave - no "atrial kick". Also, the fast rate associated with new-onset atrial fib often compromises ventricular filling and cardiac output. LBBB also has a deleterious effect on cardiac output. Wide QRS complexes indicate that the ventricles are not contracting efficiently and synchronously. The left ventricle is depolarizing by way of a slow wave of depolarization, rather than all the cells getting the message to depolarize at the same time. Having these two conditions at the same time can have a very negative effect on cardiac output, leading to CHF. The first step in treatment often involves simply slowing the rate to normal, which allows for better ventricular filling and decreases the workload on the heart. Then, the fibrillation and bundle branch block can be addressed.
There is some very slight variation in the QRS morphology in both of these ECGs. We will leave it to the more advanced Gurus to comment on this, and any other interesting features we may have missed.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Underlying LBBB with rapid AFib vs VT?
Interesting set of tracings by Dawn on a very common problem. I would like to "revisit" the premise of the 1st tracing (= ECG #1) - in which there is a fairly rapid WCT (Wide-Complex Tachycardia) without identifiable P waves. Should this be "assumed VT till proven otherwise and treated according?"
Ken Grauer, MD www.kg-ekgpress.com [email protected]