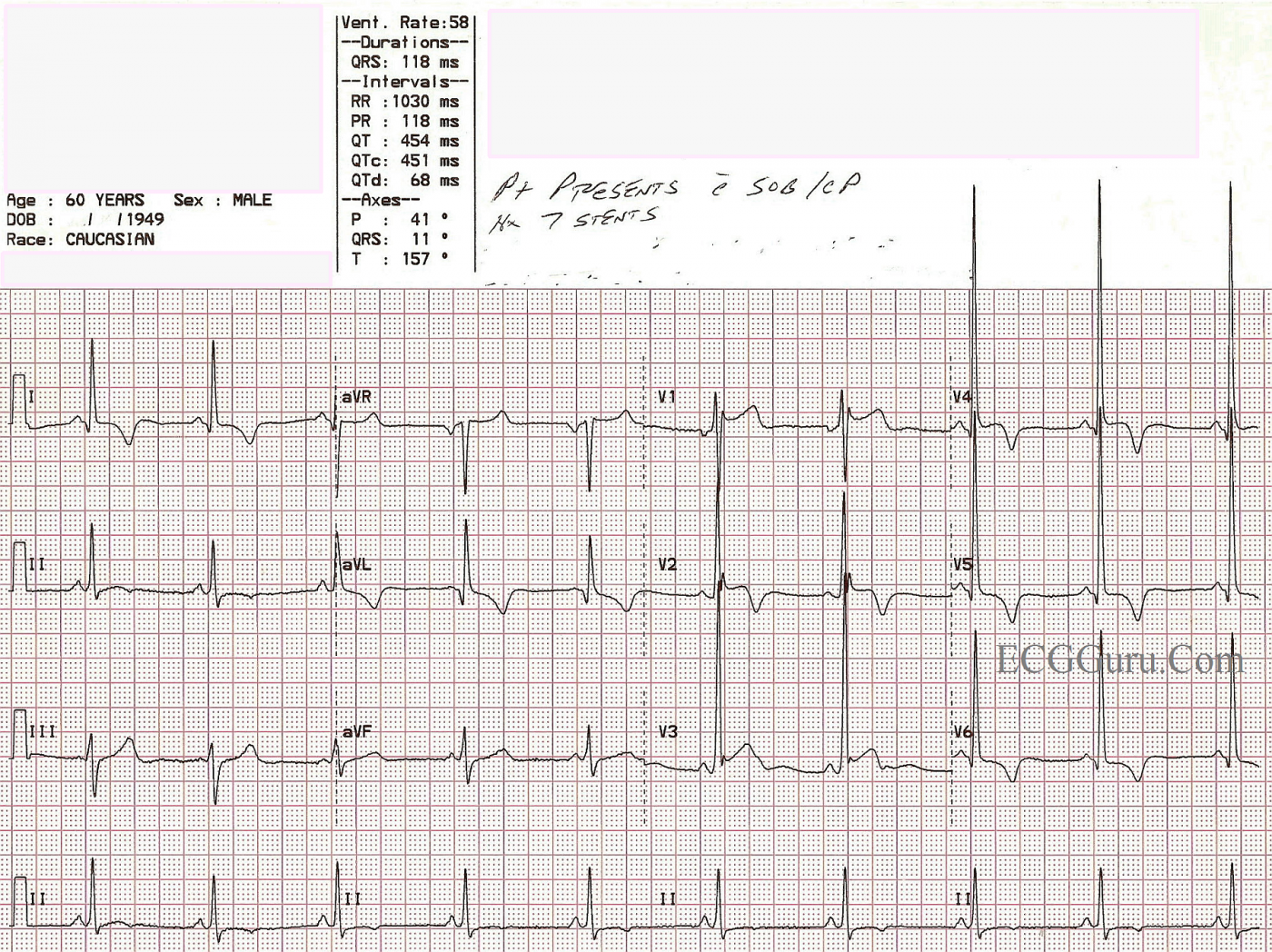
This 60-year-old man presented to the Emergency Department with chest pain and shortness of breath. He gave a history of having seven coronary artery stents in the past.
This is a good ECG for demonstrating the voltage and ST criteria for LVH and acute anterio-lateral wall M.I. in the same patient, where both conditions have been confirmed by other tests. If you are teaching the topics of ST elevation M.I., or left ventricular hypertrophy, you will probably have to address the issue that LVH can be considered a "mimic" for STEMI, especially for beginners. This is because LVH causes ST depression in leads with upright QRS complexes, and reciprocal ST elevation in leads with negative QRS complexes. This is called ST segment discordance. The ST changes in LVH are due to the "strain" pattern, indicating strain on the left ventricular myocardium. It is true that some ST elevation will appear in V1 and V2 in these patients, and can be mistaken for M.I. In the ECG shown here, the patient has definite ST elevation in leads which would NORMALLY have depression in the LVH strain pattern. Leads V3 through V6 and I and aVL have ST elevation that is not discordant, and is definitely real. In addition, the ST elevation in V1 and V2 are greater than expected for LVH alone.
The criteria most often used to determine LVH is the Sokolov-Lyon Criteria, (S wave in V1 + R wave in V5 or V6 = 35 mm). It is best to confirm the LVH with echocardiograhy.
This patient was taken to the cath lab, and the M.I. was confirmed, although his case was lost to followup, and we do not know if he received more angioplasty, coronary artery bypass, or other treatment, or what his condition was post catheterization.
For a similar ECG and discussion on this site, go to this LINK.
As always, the information presented with the Instructors' Collection series is very basic, and we welcome and look forward to comments from the ECG GURUs out there!
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
PR
Thanks for EKG, has short PR any relationship here?
Acute MI and LVH at the Same Time
Ken Grauer, MD www.kg-ekgpress.com [email protected]