All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.
Recent blog posts
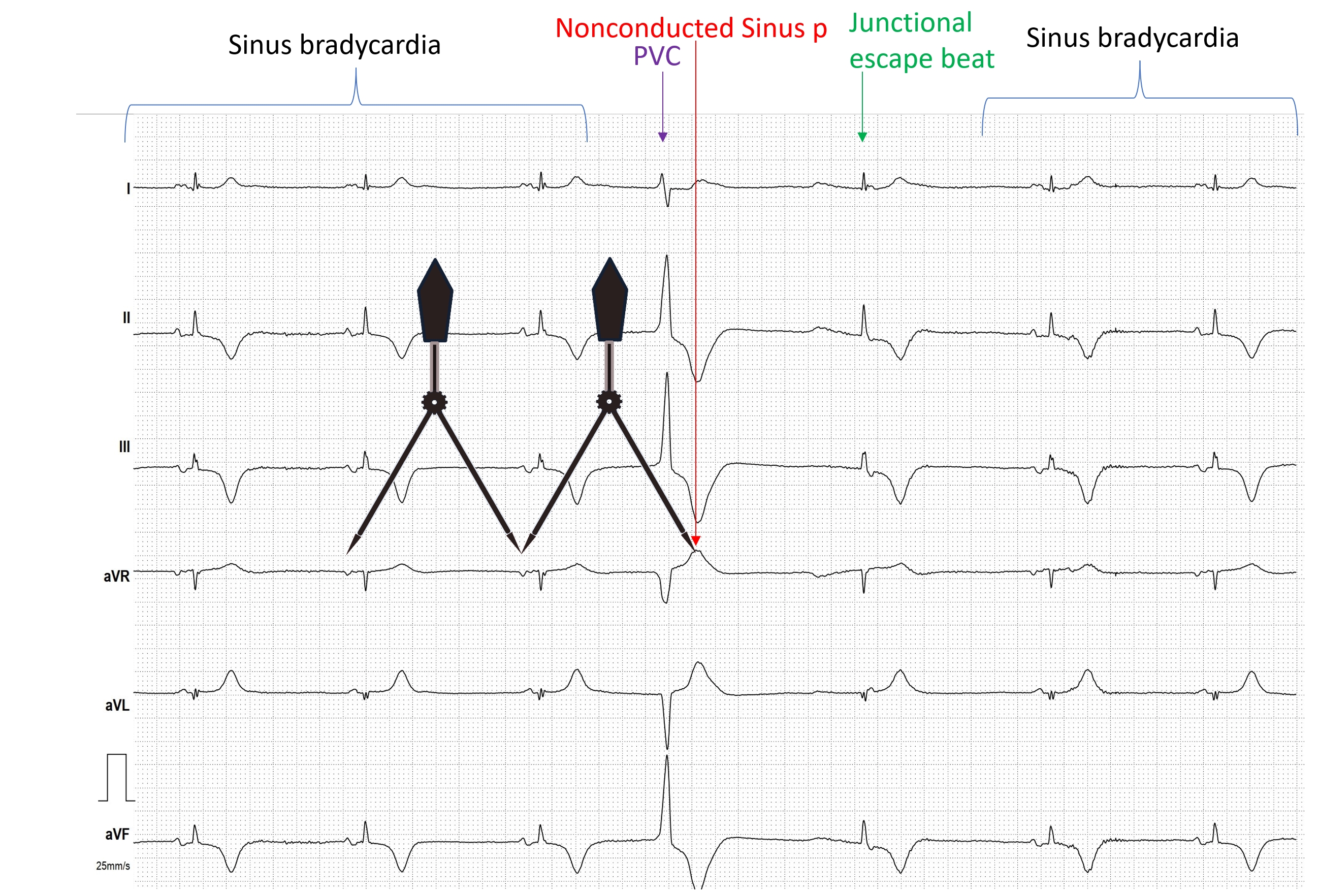
- HIGH GRADE AVB
- JUNCTIONAL ESCAPE RHYTM
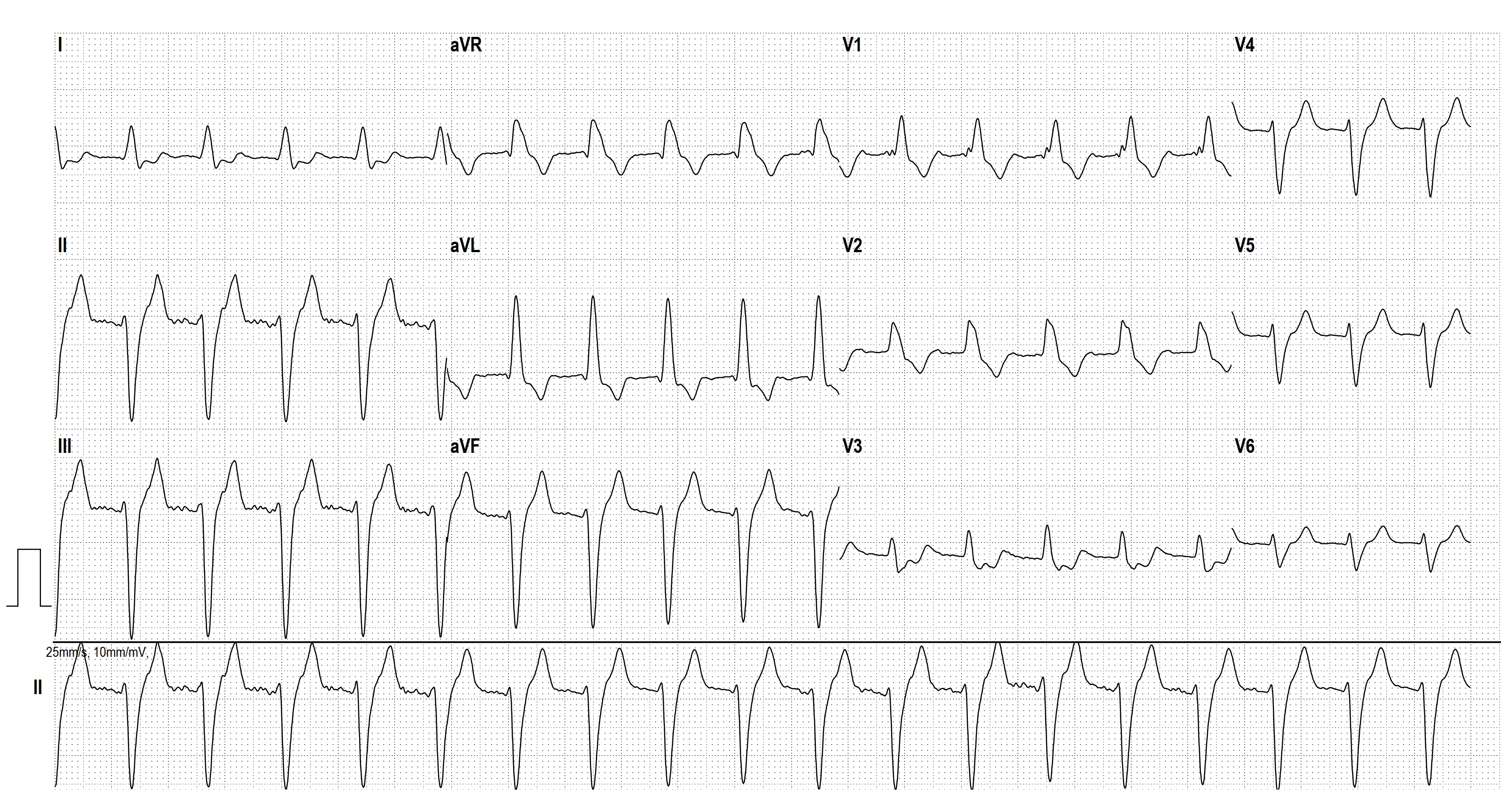
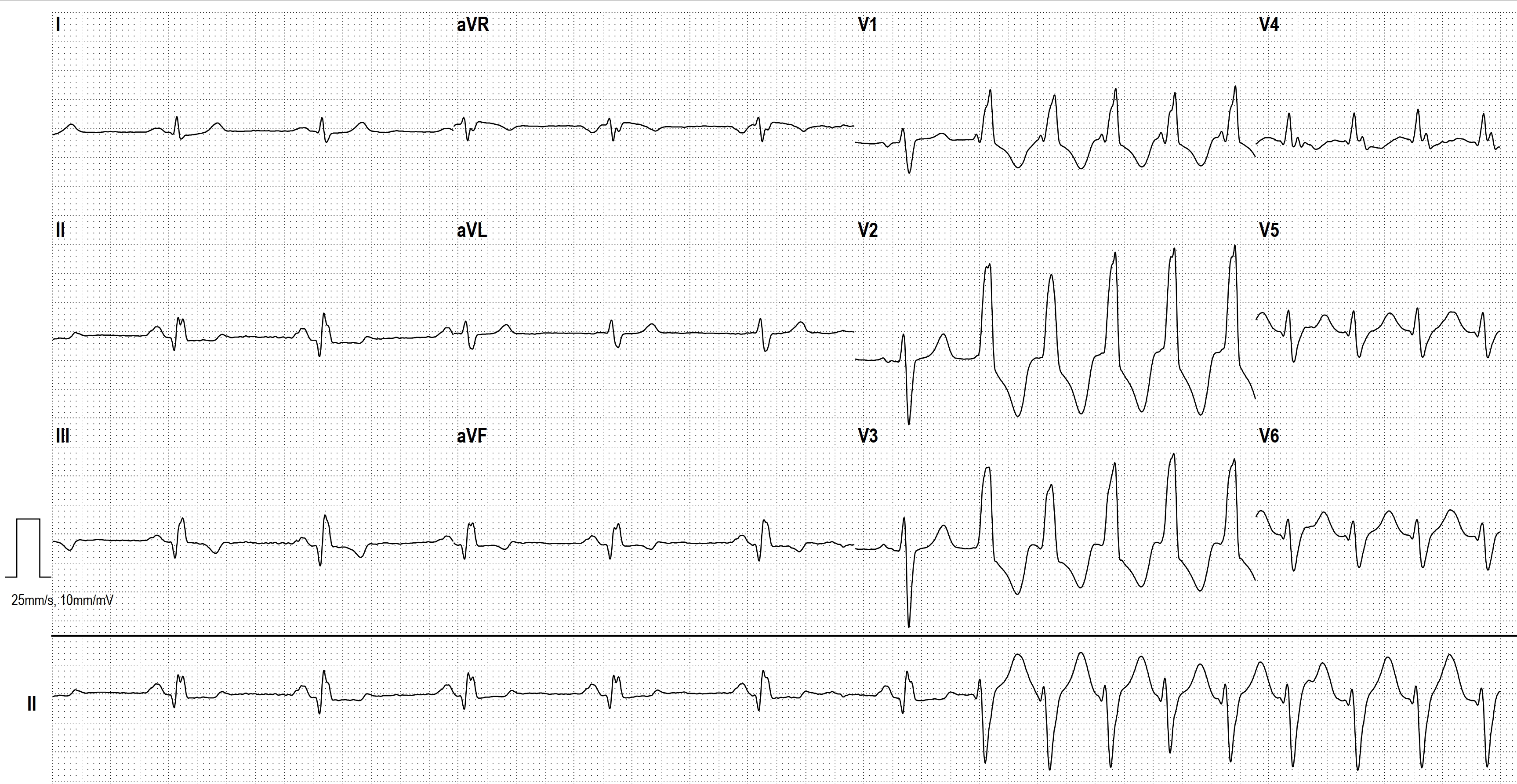
- POLYMORPHIC VT
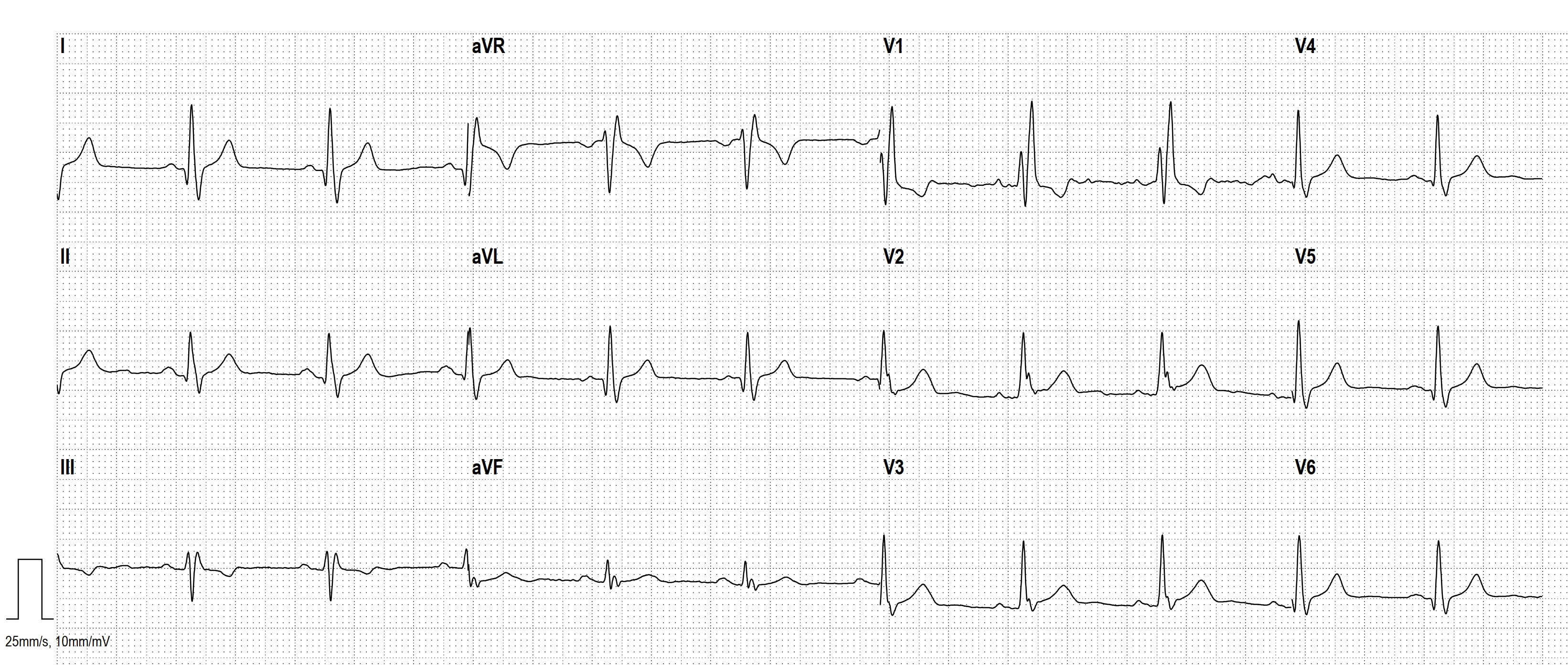
- SGARBOSSA CRITERIA
- CONCEALED CONDUCTION
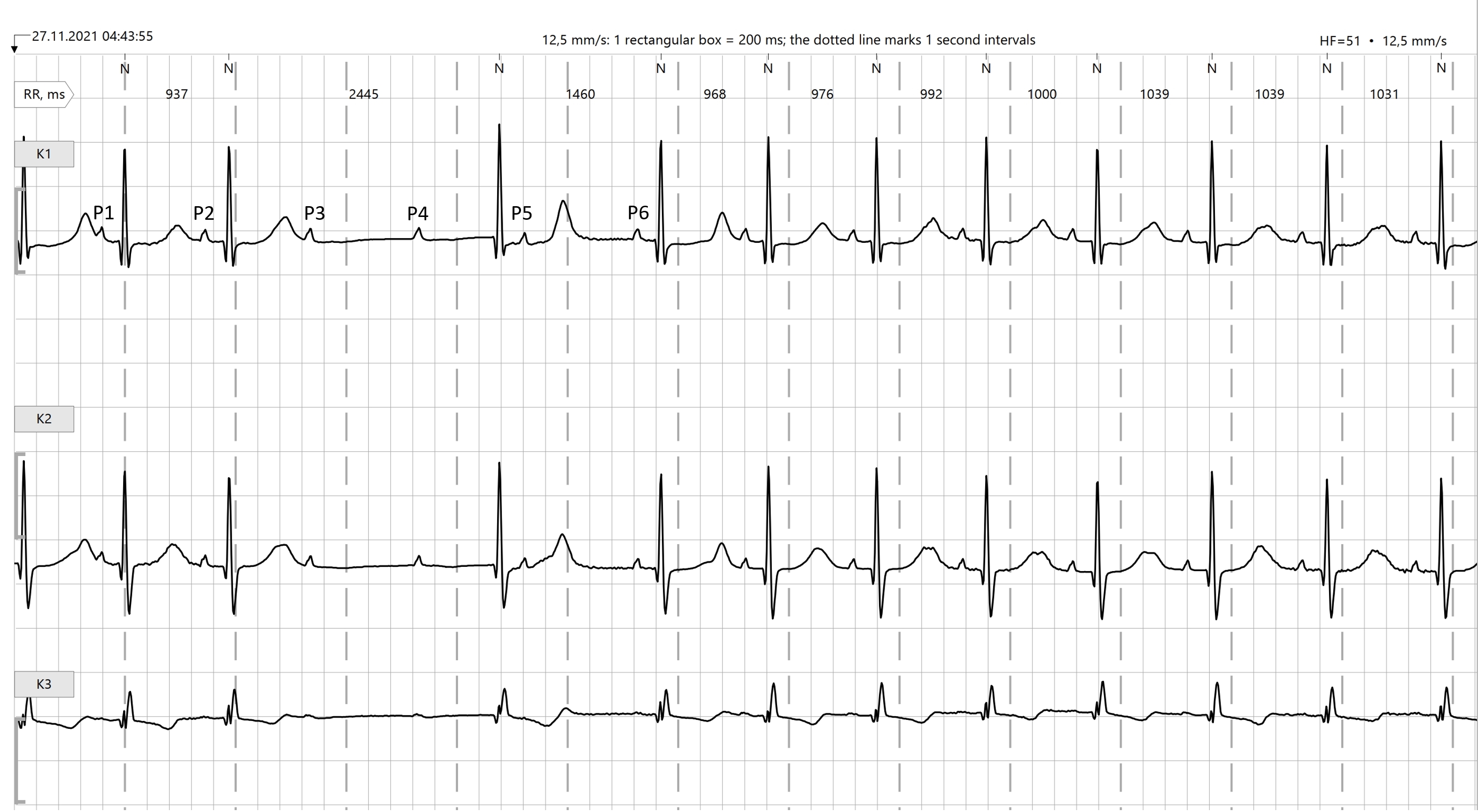
- CONCEALED CONDUCTION AND VENTRICULOPHASIC SINUS ARRHYTHMIA
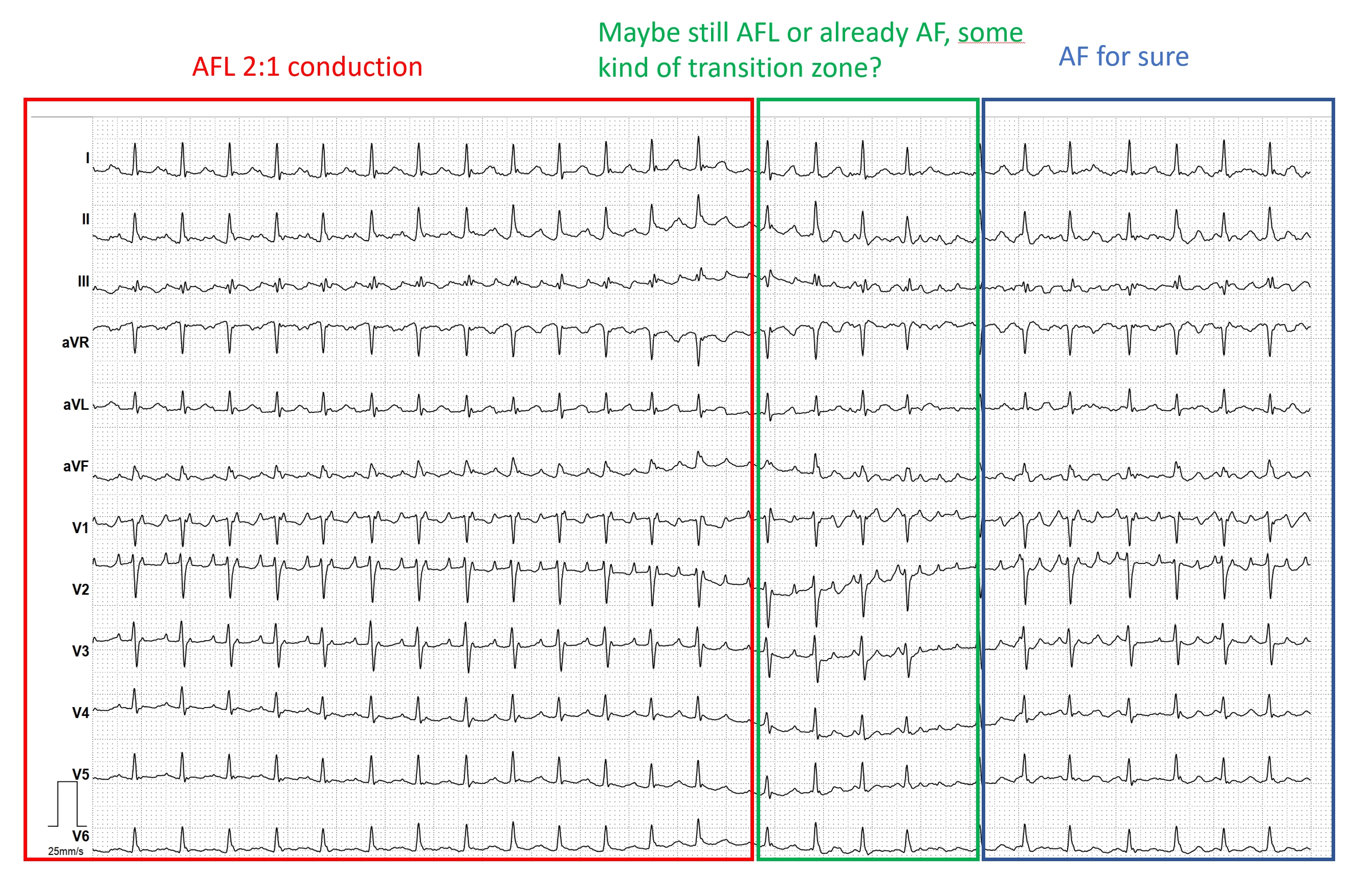
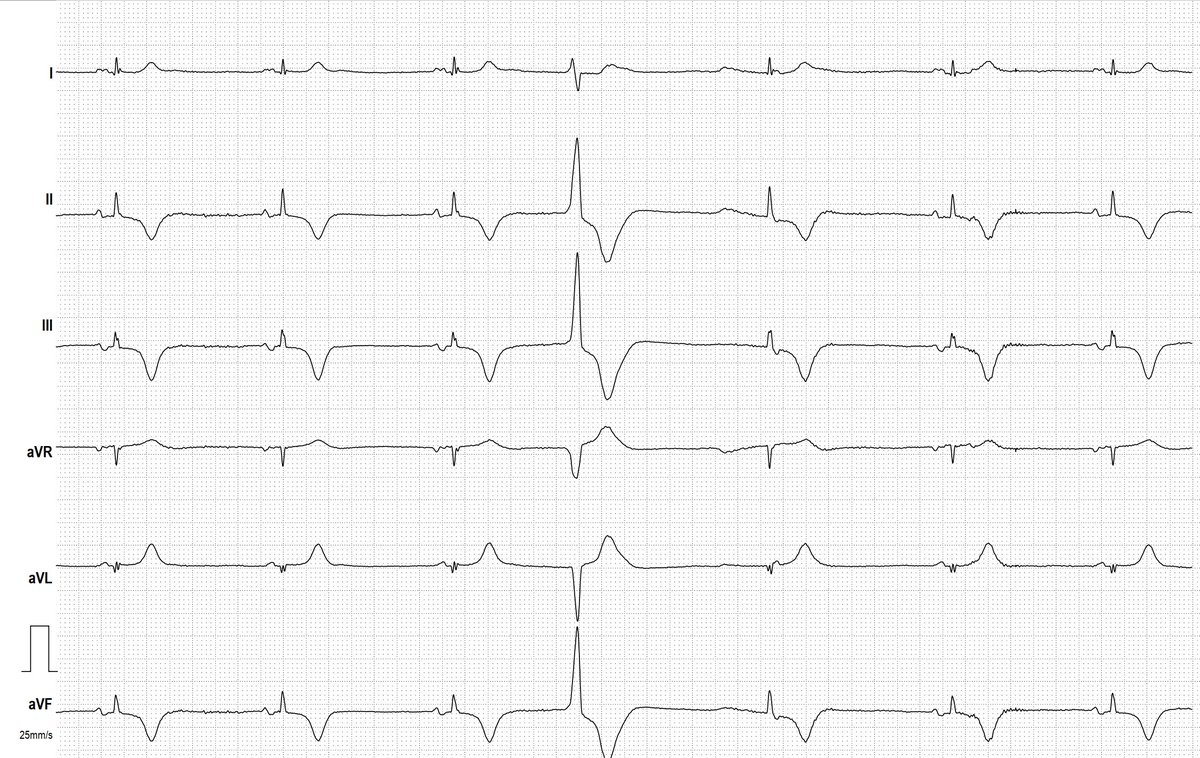
- PAROXYSMAL ATRIAL FIBRILLATION
- 2nd Degree Sino-atrial Exit Block, Mobitz Type II
- SICK-SINUS-SYNDROME
- Smartwatch Rhythm Strip
- NON-CONDUCTED PAC
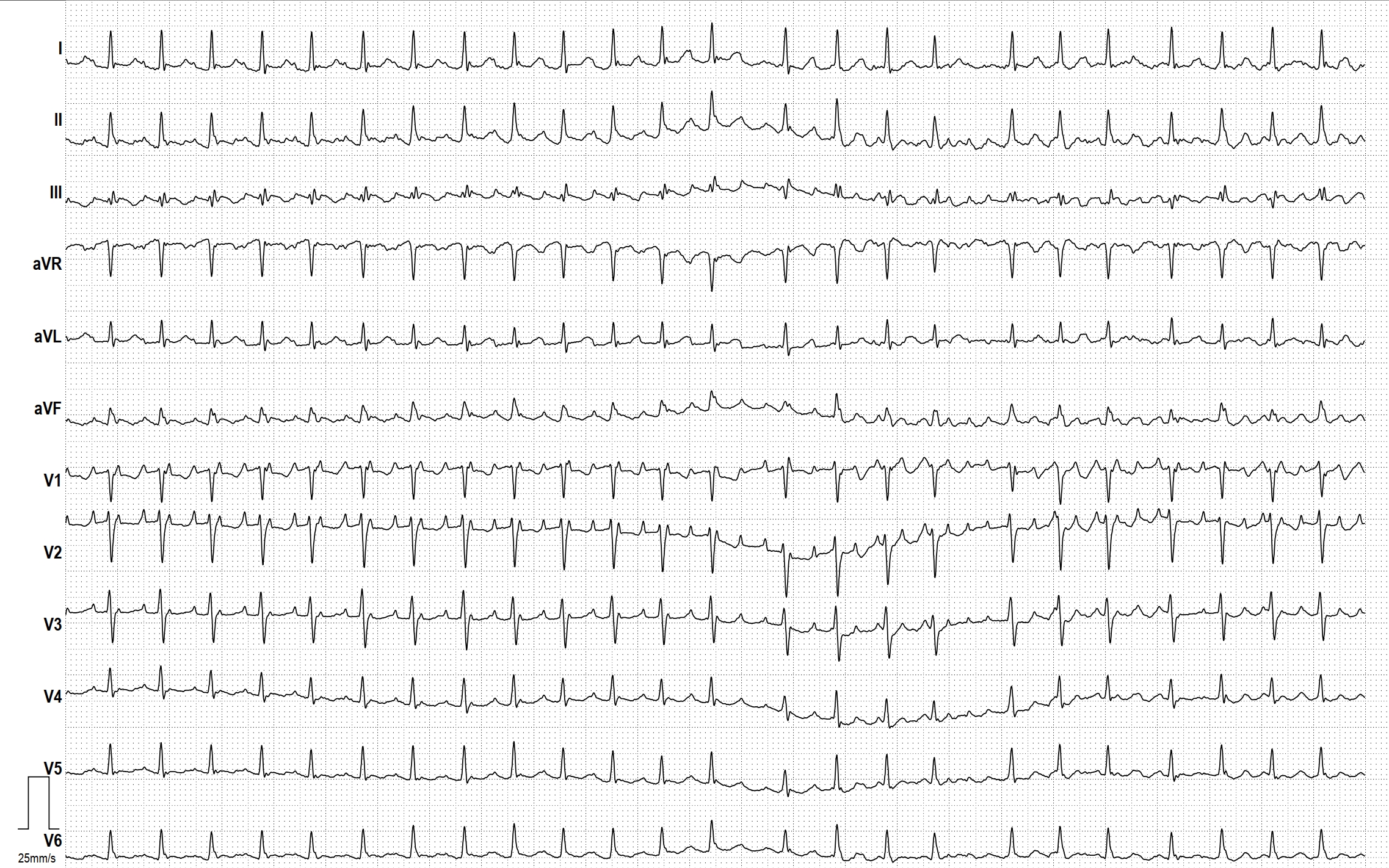
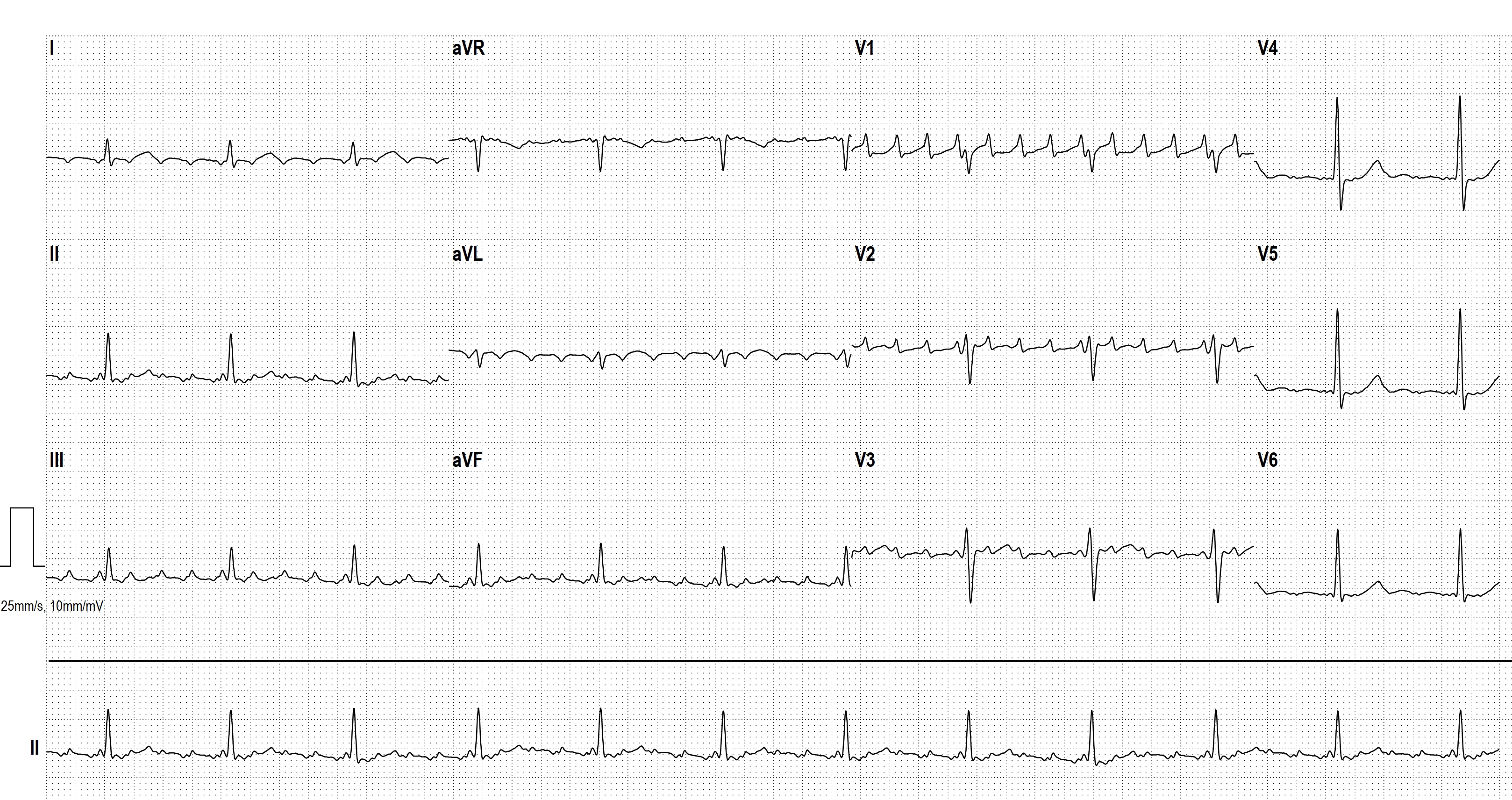
- ATRIAL TACHYCARDIA WITH PARTLY ABERRANT CONDUCTION
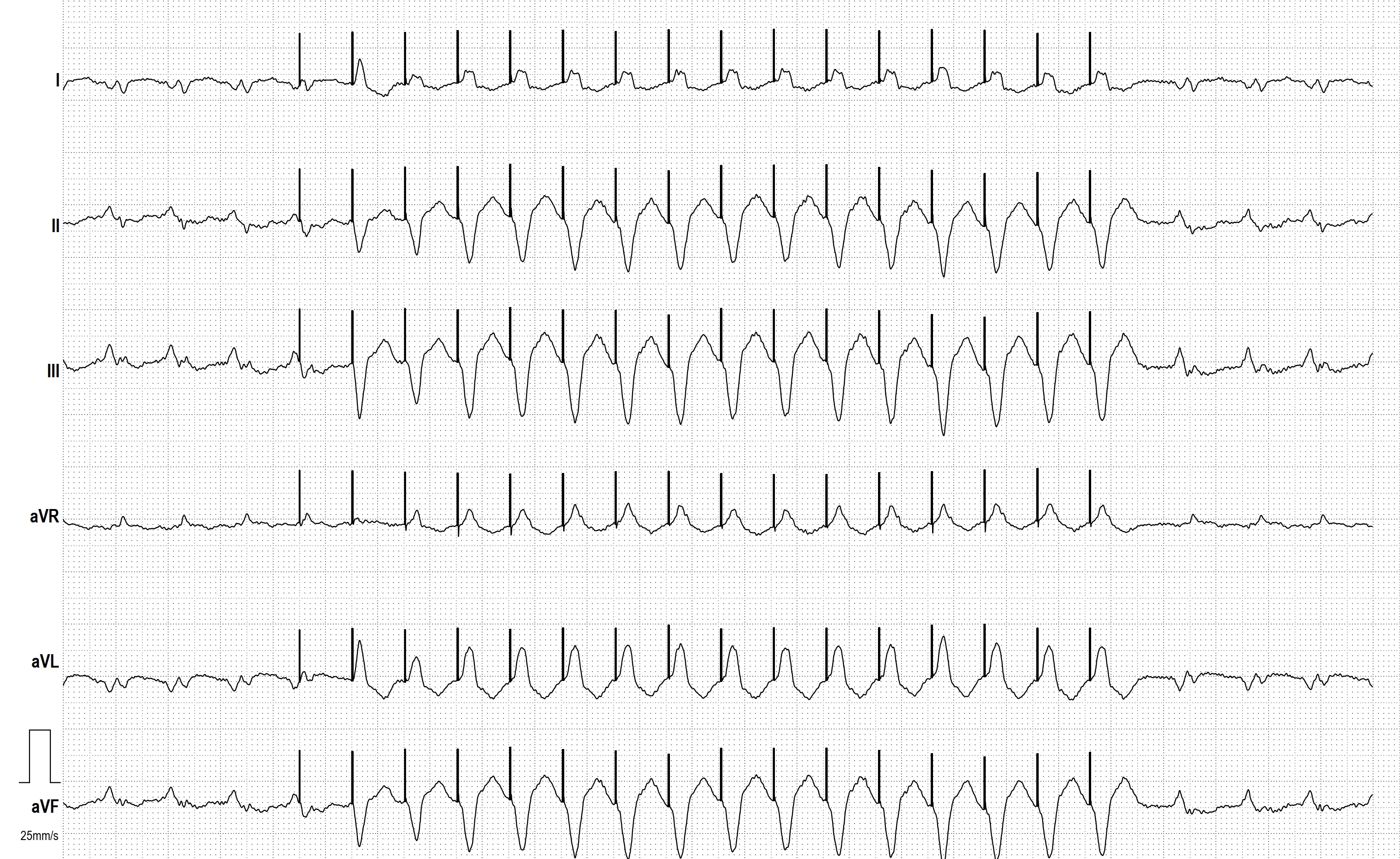
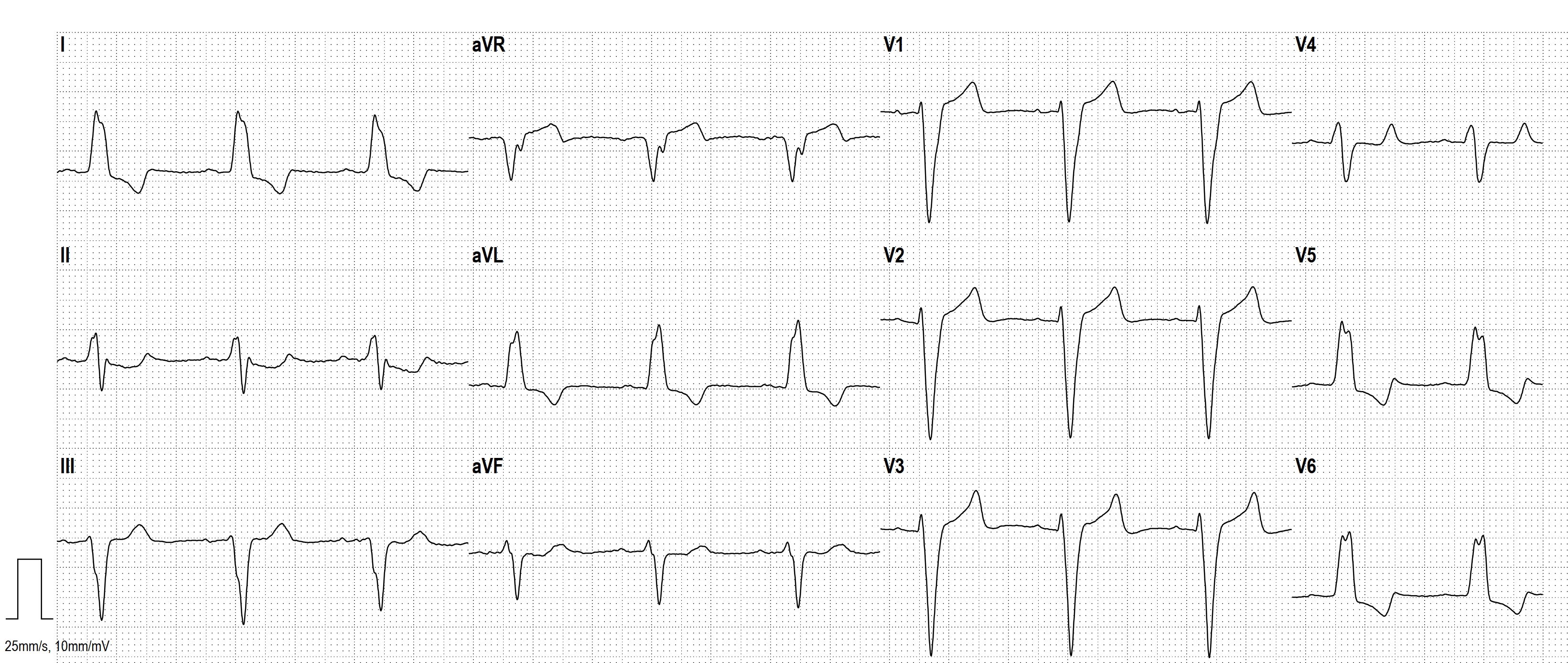
- VENTRICULAR TACHYCARDIA, ATRIAL FIBRILLATION AND ABERRANT CONDUCTION
- WHY IS THIS A PVC?
- INTERESTING HOLTER-STRIP