Question:
Dr. Jones, do you have any tips to help me teach axis determination to my students?
Today’s expert is Dr. Jerry W. Jones, MD, FACEP, FAAEM
Jerry W. Jones, MD FACEP FAAEM is a diplomate of the American Board of Emergency Medicine who has practiced internal medicine and emergency medicine for 35 years. Dr. Jones has been on the teaching faculties of the University of Oklahoma and The University of Texas Medical Branch in Galveston. He is a published author who has also been featured in the New York Times and the Annals of Emergency Medicine for his work in the developing field of telemedicine. He is also a Fellow of the American College of Emergency Physicians and a Fellow of the American Academy of Emergency Medicine and, in addition, a member of the European Society of Emergency Medicine.
Dr. Jones is the CEO of Medicus of Houston and the principal instructor for the Advanced ECG Interpretation Boot Camp and the Advanced Dysrhythmia Boot Camp.
Answer:
Frontal Plane Axis Shortcuts
When we speak of axes and vectors, we are usually referring to the mean QRS axis in the frontal plane – much more so than in the horizontal plane (where it’s more properly called “rotation” rather than “axis”). We are also concerned with the P axis and the T axis in the frontal plane. And, at times, we are even concerned with the ST (segment) axis!
That can be a lot of drawing of lines and angles and expenditure of brain power – especially after being awake and on duty most of the night. Well… relax! It doesn’t have to be difficult at all. And you don’t have to draw any diagrams!
Before we start, let’s be certain that we are speaking the same language: in electrocardiography, when we say “left” we mean the PATIENT’S “left;” when we say “right” we mean the PATIENT’s “right.” We are not referring to the right side of the diagram or ECG tracing in front of you. The positive pole of Lead I may be on the right side of the drawing of Einthoven’s triangle, but it is on the PATIENT’S left! OK, let’s proceed…
First of all there are three generalizations about axes that you should know:
FIRST, forget about axes of +23 degrees, -14 degrees or +61 degrees. You never – let me repeat – NEVER have to be so exact in electrocardiography unless you are calculating the QRS-T angle (and most healthcare providers don’t need to do that). 99 % of the time if you are within 15° to 30° of the correct mean axis you are doing JUST FINE! The reason is because 99 % of the time we just want to know if the axis is normal or not, or if it is located closer to one of the extremes of axis (the “extremes” being left axis deviation or right axis deviation). Besides, the mean QRS axis is very labile – just taking a deep breath can change it considerably!
SECOND, knowing that an axis is “normal” really doesn’t tell you a whole lot since both normal and abnormal hearts can have perfectly normal mean QRS axes in the frontal plane. However, very, very few normal hearts will have an abnormal axis. So, although knowing that the mean QRS axis in the frontal plane is normal really doesn’t help much, knowing that the axis falls outside the normal range is an extremely good indication of cardiovascular pathology.
The first axis we are concerned about is the mean QRS axis in the frontal plane. There are four leads that we use to tell us what we need to know.
First of all, to decide whether the axis is normal or not, we look at leads I and II. If the QRS is negative in I (but positive in II), then there is a right axis deviation. If the QRS is negative in II (but positive in I), then there is left axis deviation. If it is upright in both, then the mean QRS axis in the frontal plane is perfectly normal. But again – “normal” really doesn’t tell us a lot. Forget about aVF! We no longer use it in determining the mean QRS axis in the frontal plane other than to diagnose an axis in the northwest quadrant (“no man’s land”), which is very rare.
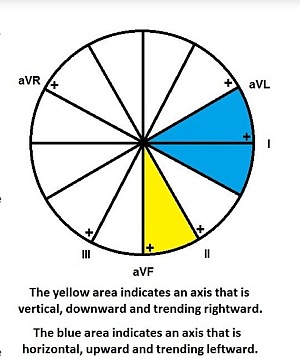
Second, we often want to know if the “normal” mean axis is tending rightward or leftward. We do that by looking at leads aVL and III. If the QRS complex is predominantly negative in aVL, then it has to be more positive than +60° (rightward). If the QRS is predominantly negative in III, then it has to be more negative than +30° (leftward). If the QRS complexes in leads aVL and III are both positive, then the mean QRS axis in the frontal plane will lie between +60° and +30° and could not be more “NORMAL!”
 Tall, thin people usually have long, elongated hearts that seem to just “hang” in their chest (and some actually do!). We would expect these individuals to have hearts that are nearly vertical, so we would also expect to see a QRS complex in aVL that is predominantly negative or maybe equiphasic. If the QRS in aVL were very positive, we would wonder about the presence of a conduction disturbance that sends the terminal depolarization upwards. (FYI, in electrocardiography, when we say an impulse is traveling “upwards,” we really mean “to the left.” If we say it’s traveling “downwards, we really mean “to the right.”)
Tall, thin people usually have long, elongated hearts that seem to just “hang” in their chest (and some actually do!). We would expect these individuals to have hearts that are nearly vertical, so we would also expect to see a QRS complex in aVL that is predominantly negative or maybe equiphasic. If the QRS in aVL were very positive, we would wonder about the presence of a conduction disturbance that sends the terminal depolarization upwards. (FYI, in electrocardiography, when we say an impulse is traveling “upwards,” we really mean “to the left.” If we say it’s traveling “downwards, we really mean “to the right.”)
Short, stocky people tend to have hearts that lie a bit more horizontally on the diaphragm, so we would expect their mean QRS axis in the frontal plane to be more horizontal. Therefore, we shouldn’t be surprised to see that lead III is predominantly negative or equiphasic.
So if we look at a 12-lead ECG and quickly see that the QRS complexes in both leads I and II are positive but the QRS complex in lead III is negative, we would say that although the mean QRS axis (or vector) in the frontal plane is normal, it is also somewhat leftward or horizontal. If the QRS in aVL were negative instead, then we would report the mean QRS axis as somewhat rightward or vertical.
Rightward means downward and leftward means upward (and vice versa, respectively).
Years ago, we were taught that any axis more negative than 0° was left axis deviation. Then, it was decided that the axis could be up to -30° and still be normal. This presented a lot of confusion regarding how to refer to a normal axis. Basically, if the mean QRS axis in the frontal plane falls between -30° and +90° call it NORMAL. If it falls between -30° and -90° call it LEFT AXIS DEVIATION. Some people still want to refer to the area from 0° to -30° as left axis deviation but with a normal axis and they do make a good argument. The issue of how to refer to that section between 0° and -30° still isn’t completely resolved.
Let’s talk about P waves. Anytime I mention “P wave axis” or “P wave vector” I usually see eyes rolling up to the ceiling. But the P wave axis is determined exactly the same way as the QRS axis!
A good pearl to remember is that any P wave axis, QRS axis or T wave axis that is located between 0° and +90° is NORMAL! Of course, a QRS axis located between 0° and -30° is also NORMAL. The vast majority of P wave axes and T wave axes are going to be found within a more narrow range within that 90° spread between 0° and +90°, but they are still NORMAL as long as they are between 0° and +90°.
That being said, we usually want to know the general direction of the P wave axis (I’m going to stop repeating “mean axis” and “in the frontal plane”). Abnormal P wave axes tend to be vertically oriented.
Normally, the P wave axis is almost parallel to the lead II axis and so it tends to cluster around +60°. A P wave in the frontal plane that is moving rightward – i.e., more inferiorly or vertically – is very characteristic of chronic lung disease such as COPD or an acute strain on the right side of the heart such as a pulmonary embolus.
If the P wave vector becomes more vertically oriented, what happens to the P wave in lead I? Lead I is perfectly horizontal on the Einthoven triangle, so if the P axis is vertical, then it must be perpendicular to lead I. When a vector is perpendicular to a lead it can be either isoelectric or equiphasic. In the case of the P wave, it is usually isoelectric – or nearly so. In any case, a P wave with a vertical axis will be very small or totally isoelectric in lead I. Obviously, we normally do see P waves in lead I so equally obviously the P wave axis is usually not particularly vertical.
The T wave axis can be handled exactly the same way as the QRS and P wave axes. However, we really don’t look at the T wave axis that much. When we do, it’s usually in reference to the angle formed between the T wave axis and the QRS axis (on the hexaxial reference grid) called the QRS-T angle. In calculating the QRS-T angle, we really do want to use axes that are as accurate as possible. However, determining those axes to the nearest degree isn’t really as difficult as you might imagine. Here’s my method:
I use the R and T axes printed on the ECG printout. Seriously… this is how 98% of all physicians calculate the QRS-T angle (and the other 2% are liars!).
Joking aside, advanced electrocardiographers do sometimes use the T wave axis to interpret 12-lead ECGs, but most healthcare providers need only note that the T wave is inverted in certain leads under certain conditions.
I said there were three generalizations about axes, so here’s the third…
THREE, most healthcare providers reading ECGs at a beginners’ or low-intermediate level tend to focus on positive deflections and really don’t pay that much attention to negative deflections (except for Q waves and deeply inverted T waves). But there’s a lot of information to be gathered from negative deflections.
Let’s focus on S waves. Let’s say we are dealing with a heart that has a nearly vertical QRS axis with predominantly negative QRS complexes in leads II, III and aVF. That means that the ventricular depolarization is heading straight up. But what if the deepest S wave is in lead III? That would tell us that the preponderance of the electrical force is pointing up and to the left (around -60° and parallel to the lead III axis) which would point to the basal-lateral area of the left ventricle. Therefore, we likely have a heart with a problem in the left ventricle – perhaps in the area served by the LAD, LCx or ramus intermedius. One would also like to see what’s happening in lead aVL because it’s up in that area also. Usually the problem will be LVH or LAFB (anterior hemiblock). And what if lead II has the deepest S wave? That would indicate that the QRS axis is likely parallel (or nearly so) to lead II and traveling away from its positive pole which would be up and to the right (around -120°) – likely a problem in the right ventricle or the RCA circulation. If that were the case, one would want to look at lead aVR because it’s up there in that vicinity, too.
Just remember that when we speak of positivity or negativity of a deflection in any of the frontal leads, we are talking about vertical or horizontal axis. Positivity or negativity in lead I is considered the “gold standard” for determining “rightwardness” or “leftwardness,” but it often really isn’t that useful for the simple reason that it is rather unusual to see predominantly negative complexes in lead I. That’s because axes in the frontal plane are typically normal. So we have to look at other leads that indicate a rightward tendency or leftward tendency within the context of a normal axis and those leads are lead III (negativity indicates “leftwardness”) and lead aVL (negativity indicates “rightwardness”). The inferior leads – II, III and aVF – indicate verticality (downward or rightward if positive, upward or leftward if negative).
So, in the final analysis, you usually just want to know if you have a vertical axis or a horizontal axis, if the axis is outside the limits of normality and occasionally, when the axis is normal, you may want to know if it is trending leftward or rightward. Now you know how to determine this information without doing any diagraming or calculating.