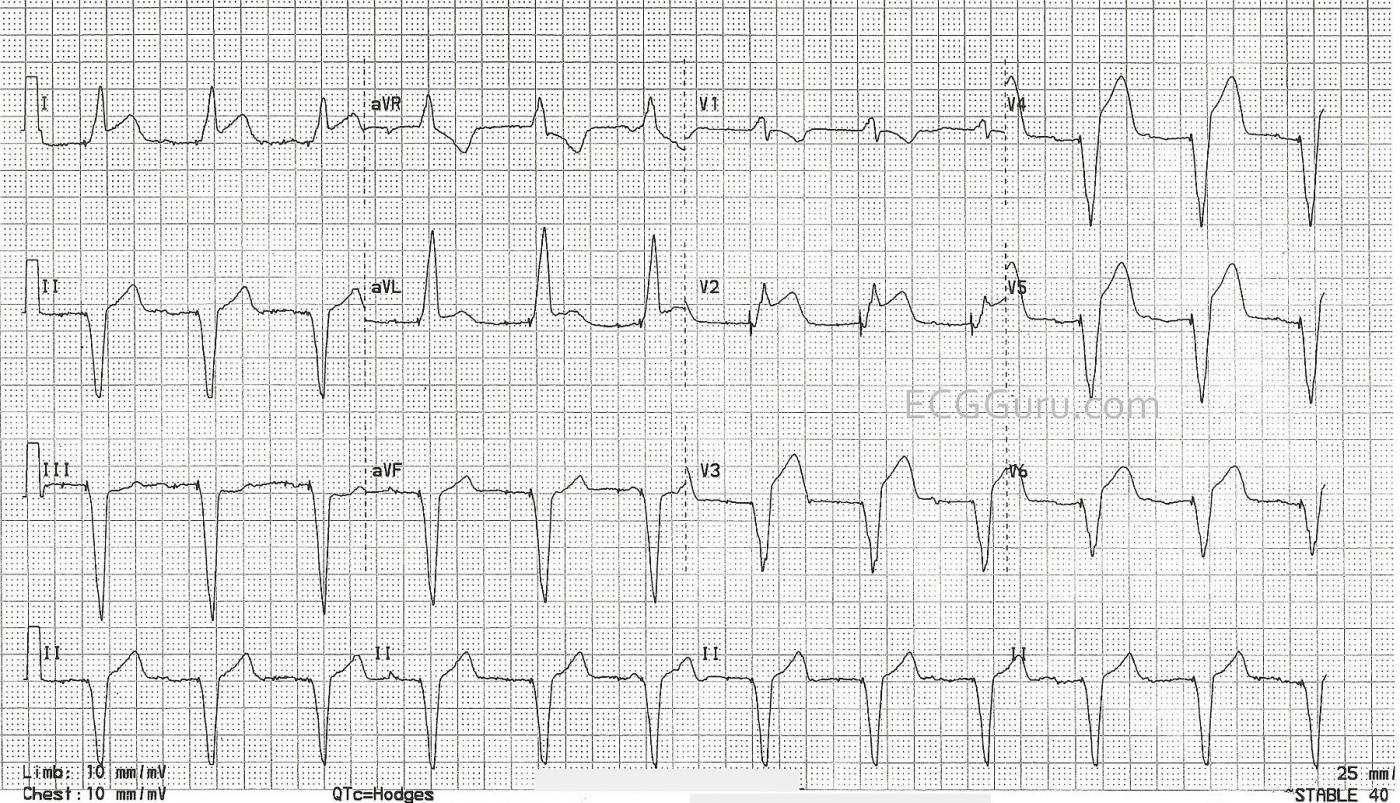
This ECG is taken from an elderly man who has a history of complete heart block and AV sequential pacemaker. On the day of this ECG, he presented to the Emergency Department with chest pain and shortness of breath. His vital signs were stable and within normal limits. We do not have information about his treatment or outcome.
I don’t see spikes. How do we know this is a paced rhythm? The ECG clearly shows the presence of an AV pacemaker. There are very tiny pacer “spikes”, probably best seen in Leads III, aVF, aVL, and most of the precordial leads. Other ECG signs that this is a paced rhythm are: wide QRS at about .16 seconds (160 ms); abnormal left frontal plane axis; regular rhythm with AV dissociation (there are P waves seen occasionally that have no fixed relationship to the QRS complexes). Also, V6 is negative. That rules out left bundle branch block unless the electrodes are misplaced. There are no capture beats in this strip. The patient appears to be, at least right now, 100% dependent on the paced rhythm.
Why does the presence of a pacemaker make it harder to diagnose an M.I. from the ECG? Wide-QRS rhythms, such as right-ventricular paced rhythms, left bundle branch block, and ventricular ectopic rhythms, usually have “discordant ST and T wave changes”. That is, when the QRS is positive (upright), the ST and T wave are negative. The reverse is also true: when the QRS is negative and wide, the ST and T wave changes are positive (ST elevation). This is not true for right bundle branch block because the conduction delay that causes the widening of the QRS is in the right ventricle, and the ST segment is reflecting the LEFT ventricle’s repolarization. Discordant ST changes can make it difficult to determine from the ECG alone that there is an ST elevation M.I. (STEMI). Diagnosis usually must be made from patient presentation, ECG changes over time, and cardiac enzymes – or more definitively from cardiac angiogram. Pacemakers that produce narrow QRS complexes do not cause discordant ST changes.
Can we see an M.I. on this ECG? Remember that this patient was complaining of chest pain. Fortunately, his STEMI is pretty easy to see on the ECG. He has ST ELEVATION in leads where there should be ST depression. That is, the wide-QRS complex paced rhythm has POSITIVE QRS complexes in Leads I and aVL – he should have ST DEPRESSION from the paced rhythm. Instead, he has ST ELEVATION. This is anterior-lateral STEMI. Lead III shows ST depression where we would expect to see elevation. This is a reciprocal change caused by the M.I. Also, Leads V2 through V6 have ST ELEVATION that is more pronounced that one would expect from a paced rhythm alone.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Paced Tracing showing Acute STEMI
I essentially agree with comments by Dawn. Pacing spikes are clearly seen in many (most) leads. Pacing changes the sequence of ventricular activation — therefore both depolarization and repolarization sequences are altered — which is why assessment for acute ischemia infarction is usually so difficult. And there are just so many types of pacemakers that can be placed at various sites in the heart that we just don’t have predictable millimeter “guidelines” the any specific amount of abnormal ST-T wave changes. But as per Dawn — leads I, aVL and V2 definitely show abnormal ST elevation that in association with the history of new-onset chest pain is diagnostic of an acute STEMI. In this context — there IS subtle (but real) reciprocal ST depression in lead III — and the amount of J-point ST elevation in V3-thru-V6 is just “more-than-it-should-be”, even when you have a paced rhythm. KEY — Rather than any “formulas” — I put great value on the history (ie, Was there new-onset chest discomfort?) — and on qualitative assessment of leads that show ST-T wave morphology shapes that just should not be. That’s why in this tracing, even though the patient has a pacemaker — the ST elevation in leads I, aVL and V2 is diagnostic of an acute STEMI.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Atrial pacing failure?
I know that key issue here is an MI in someone with a paced rhythm, but I wonder if there is another issue, albeit of lesser importance. The patient has a dual chamber pacemaker, yet, as Dawn points out, there are dissociated P waves. This should not be the case. There is no doubt that the pacemaker is producing atrial and ventricular pacing spikes in sequence these can be seen in the inferior leads and I have shown a section of aVF (lower strip) with the atrial pacing spikes highlighted by arrows. I can see no evidence of atrial capture following these spikes and in some of the leads there do appear to be independent P waves which, had they been sensed, would have inhibited atrial pacing and triggered ventricular pacing. I have placed a short strip of V4 immediately above the aVF strip and pointed out what appear to be native P waves. This all suggests that in addition to the MI, there is failure of atrial sensing and capture.
Dave R