To continue on a topic started by Jason Roediger in his February ECG Challenge -
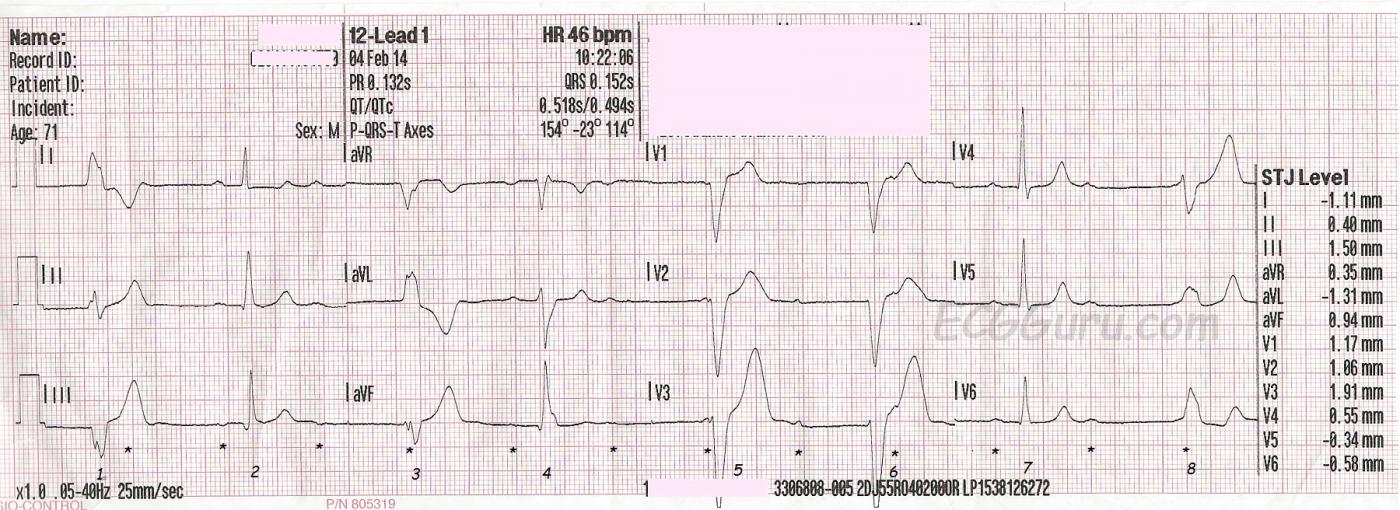
This series of two ECGs was taken from a 71-year-old man who complained of dizziness and near-syncope the day before these ECGs were done. He was seen in an Emergency Dept., and advised to follow up with a neurologist. On the day of these ECGs, still feeling dizzy and like he would pass out, he called EMS again. He denied chest pain. We do not know his past medical history. The first ECG was taken at 10:22 am. His BP was 177/76 and SpO2 99%. It shows a regular sinus rhythm (p waves marked by small asterisks) at a rate of about 75 / min. There is a high-grade AV block, meaning that some P waves are conducted (beats 2, 4, 7), but most are not. In addition, he has an escape rhythm, probably ventricular, at a rate of just over 40 / min. The overall effect of the escape rhythm is to keep the heart rate above 40 beats per minute.
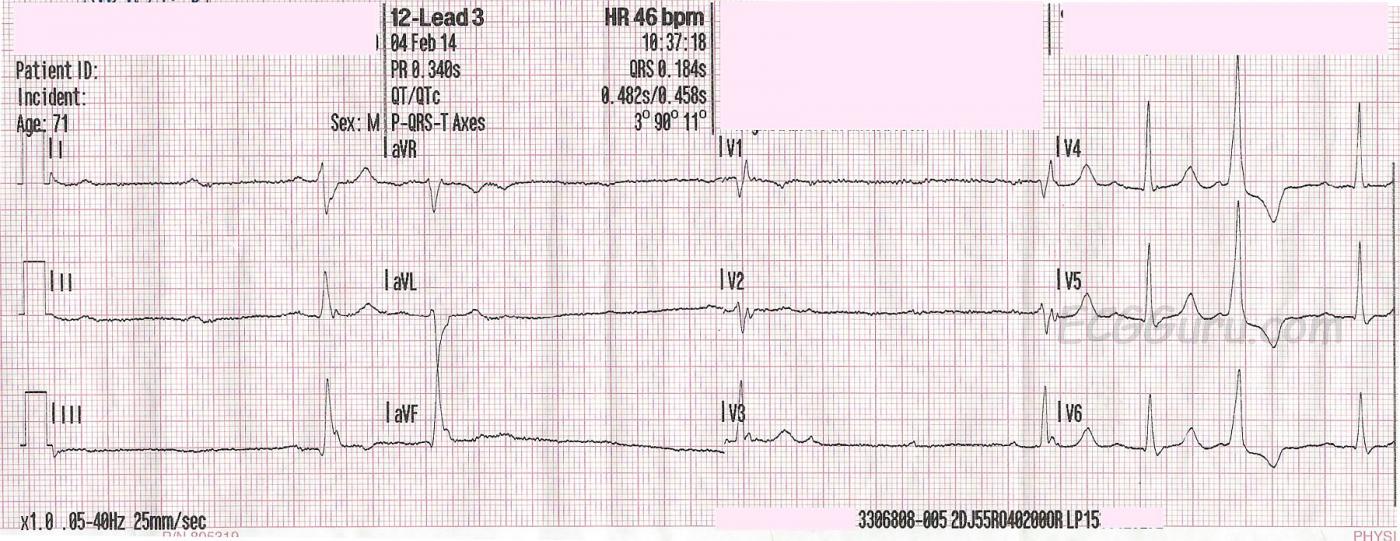
Fifteen minutes later, at 10:37 am, another ECG is taken. The patient's BP is 154/86. This ECG shows the high-grade AV block quite well, but this time, most of the QRS complexes on the strip are conducted from P waves. It is difficult to see all the P waves in every lead, but if you remember that all three channels are run simultaneously, you will find evidence of the P waves in at least one of the three leads represented at any given time. (Example: V1, V2, and V3 - V3 shows the P waves well). The next-to-last QRS on the page is interesting, as it has a different PRI than the normally conducting beats. Is this a fusion beat or an aberrantly-conducted one? It probably does not matter to the outcome of the patient.
The slowing of the rate in the second strip gives us a clue as to why the patient felt dizzy, but the blood pressures recorded did not catch hypotension. Possibly if the patient had been standing instead of lying on a stretcher, we would have seen more hemodynamic changes.
Unfortunately, we do not know the outcome of this patient, but it seems he is a candidate for an implanted pacemaker.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
High-Grade AV Block in a 71yo with Multiple Dropped Beats
Agree completely with Dawn’s interpretation of these 2 serial tracings. I’d add several points.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Thank you, this answered my
Thank you, this answered my question.