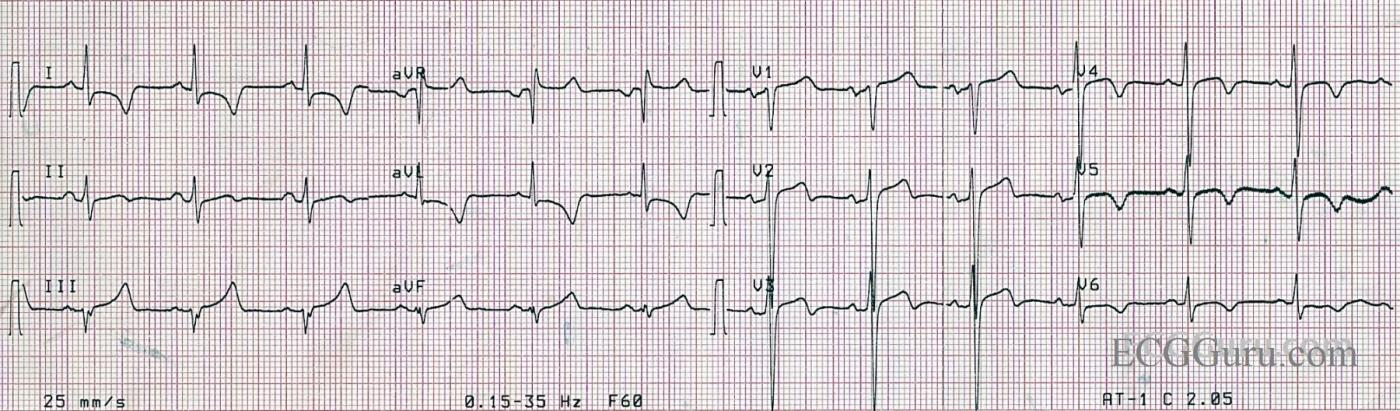
This is a very interesting ECG taken from an acute M.I. patient. Your basic level students will be able to appreciate the ST elevation in V1 through V3. Although the elevations are not very high, there are plenty of other abnormalities that point to acute STEMI: the ST segments are flat and there are marked ischemic T waves in the lateral leads: V4 through V6 and I and aVL. The patient was suffering an acute episode of chest pain.
It is also noticeable that R wave progression in the precordial leads (V1 through V6) is not optimal, as there is still a significant S wave in V6. We do not know if this is an electrode placement issue or not. The QT interval is just at the high limit of normal.
For your more advanced students, aVR has ST elevation. It is not reciprocal of an ST depression in Lead II. Research has shown that ST elevation in aVR and V1, especially when the ST elevation is greater in aVR, is a strong indication of proximal LCA or a Left Main occlusion. Unfortunately, we do not have cath results for this patient. In acute M.I. patients, higher mortality rate has been associated ST elevation in aVR.
For more information about ST elevation in aVR, click here: https://login.medscape.com/login/sso/getlogin?urlCache=aHR0cDovL3d3dy5tZWRzY2FwZS5jb20vdmlld2FydGljbGUvNTg5Nzgx&ac=401
and here: http://content.onlinejacc.org/cgi/content/full/38/5/1355
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Anterior MI — with MANY Interesting Associated Features
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Not straightforward...
I think this is an interesting and difficult ECG. As Ken says, there is evidence of LVH and this makes interpretation of the ST segments and T waves a little more complicated: some - though certainly not all – of the ST depression/elevation and T wave inversion may be attributed to LVH. I agree with Ken that the terminal T wave inversion is Wellens-like, so perhaps the patient had a partial LAD occlusion or tight LAD stenosis, rather than a complete occlusion, with widespread subendocardial ischaemia. Dawn’s assertion that the ST elevation in aVR is not reciprocal is interesting to consider because I find it very difficult to say whether it is the ST depression or the ST elevation in the limb leads that is the primary change. My suspicion is that the ST depression in I and aVL is the primary change, representing ischaemia, and that the ST elevation in III (1 mm) and aVR is reciprocal to this. It is a mathematical necessity that if on average there is ST depression in I and II, there will be ST elevation in aVR. On the other hand, as Ken points out, there may have been an occluded ‘wraparound’ LAD with consequent anterior and inferior infarction. Although it widely held that ST elevation in aVR is indicative of left main occlusion, I know that Dr Stephen Smith states that that this feature is actually due to left main insufficiency, not occlusion, with consequent global subendocardial ischaemia (and widespread ST depression). I believe he says that patients with a completely occluded left main rarely live long enough to have an ECG recorded, but when they do it shows widespread ST elevation. It’s a great shame that we don’t have cath results here because I think there are a few plausible interpretations of this very interesting ECG.
Dave R
There is More that We Don't Know (than What We Know ... ).
Ken Grauer, MD www.kg-ekgpress.com [email protected]
no disagreement
Ken - I agree with all you say! It's all very intriguing.
Dave R
Great discussion
Thanks, Dave and Ken, for the great discussion. I regret that I have so many great ECGs in my collection that don't have good clinical information. This is a "field" ECG that was given to me by a paramedic, and, unfortunately, I only recorded that it was from a "chest pain" patient who was diagnosed with an M.I. Considering the fact that it is an EMS ECG (only 3 channels) we know it was taken earlier than the diagnosis.
I have a very bad habit of using the word "occlusion" when I mean "lesion" - which could result in partial or complete occlusion. I completely agree with you, Ken, that a total LM occlusion would provide a much more dramatic ECG (briefly) or none at all, as that is usually a rapidly fatal lesion. I really need to work on this bad habit.
Thank you both for the stimulating discussion. I always learn a lot from both of you.
Dawn Altman, Admin