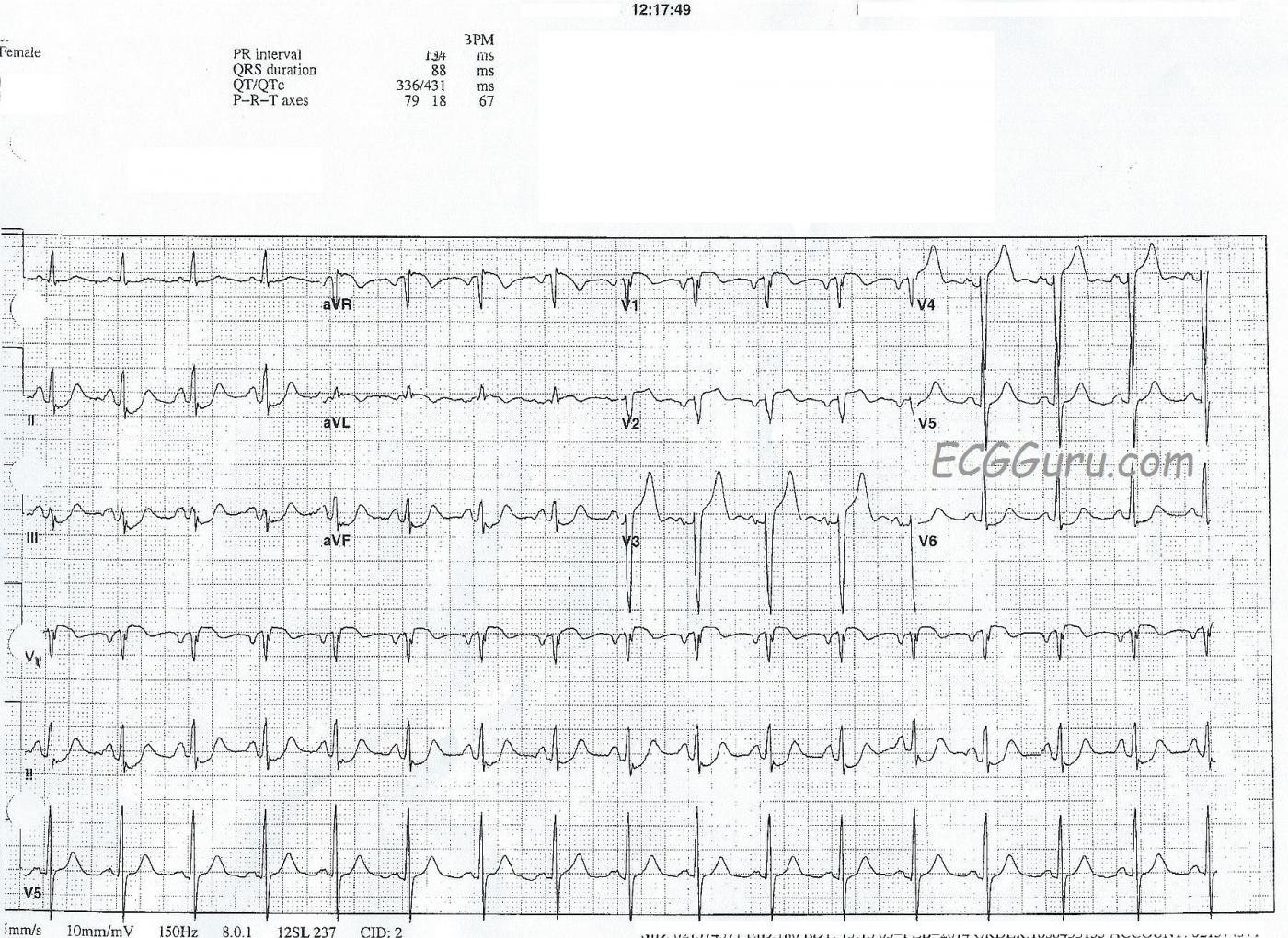
A 78-year-old woman complained of nausea and diaphoresis. Paramedics in the field found that her 12-lead ECG showed ST elevation in V1 through V4, aVL, and aVR. The patient denied chest pain and also denied any cardiac history. She did not want to be transported to the hospital, but thankfully, the paramedics understood that this was not an option, and convinced her to go.
She was taken to a cardiac facility as a STEMI Alert, was evaluated in the cath lab, and sent immediately to the O.R. for coronary artery bypass surgery. She had severe multi-vessle disease and a lesion in her proximal left coronary artery. No other details of the cath results are known.
Some important teaching points:
- there is subtle ST elevation in V1 and V2, but the SHAPE of the ST segment is suspect, with flattening and almost a coving upward shape in V1. Normal ST segments are convex downward, like a smile.
- there is nearly complete loss of r waves in V1 and V2, and V3 and V4 have very small r waves. This signals impending pathological Q waves, a sign of necrosis of the myocardium. Necrotic muscle does not contract.
- there is slight ST segment elevation in aVR. Along with STE in V1, this is a marker for proximal LCA or left main occlusion.
- the ST elevations in V3 and V4 are more pronounced, and easily meet STEMI guidelines: currently 1.5 mm of elevation in V3 and 1 mm of elevation in V4 for a woman.
- there are reciprocal ST depressions in II, III, and aVF - common in AWMI.
- aVL has slight STE, along with inverted T waves. Somewhat surprisingly, there is no ST depression in Lead I. This indicates high lateral wall injury.
- the patient has a "hint" of the criteria for LVH: her S wave in V3 + her R wave in V5 = about 33 mm, and there is depression in V6. A stretch to call it "LVH", but possibly a sign of left ventricular strain because of the acute M.I.
- there are atrial abnormalities suggested by the tall, peaked P waves in Lead II, the "M" shaped P waves in Lead III, and the inverted P waves in V1 and V2. Possibly bi-atrial dilation and stress brought on by the M.I.? An echocardiogram would be a better test for this.
- the heart rate, at about 90 bpm, reflects NSR but is a cause of more stress on an overworked, injured heart.
This is a great teaching ECG, and we hope the Gurus out there will add even more interesting points to consider.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Anterior Infarction and Other Stuff ....
Ken Grauer, MD www.kg-ekgpress.com [email protected]