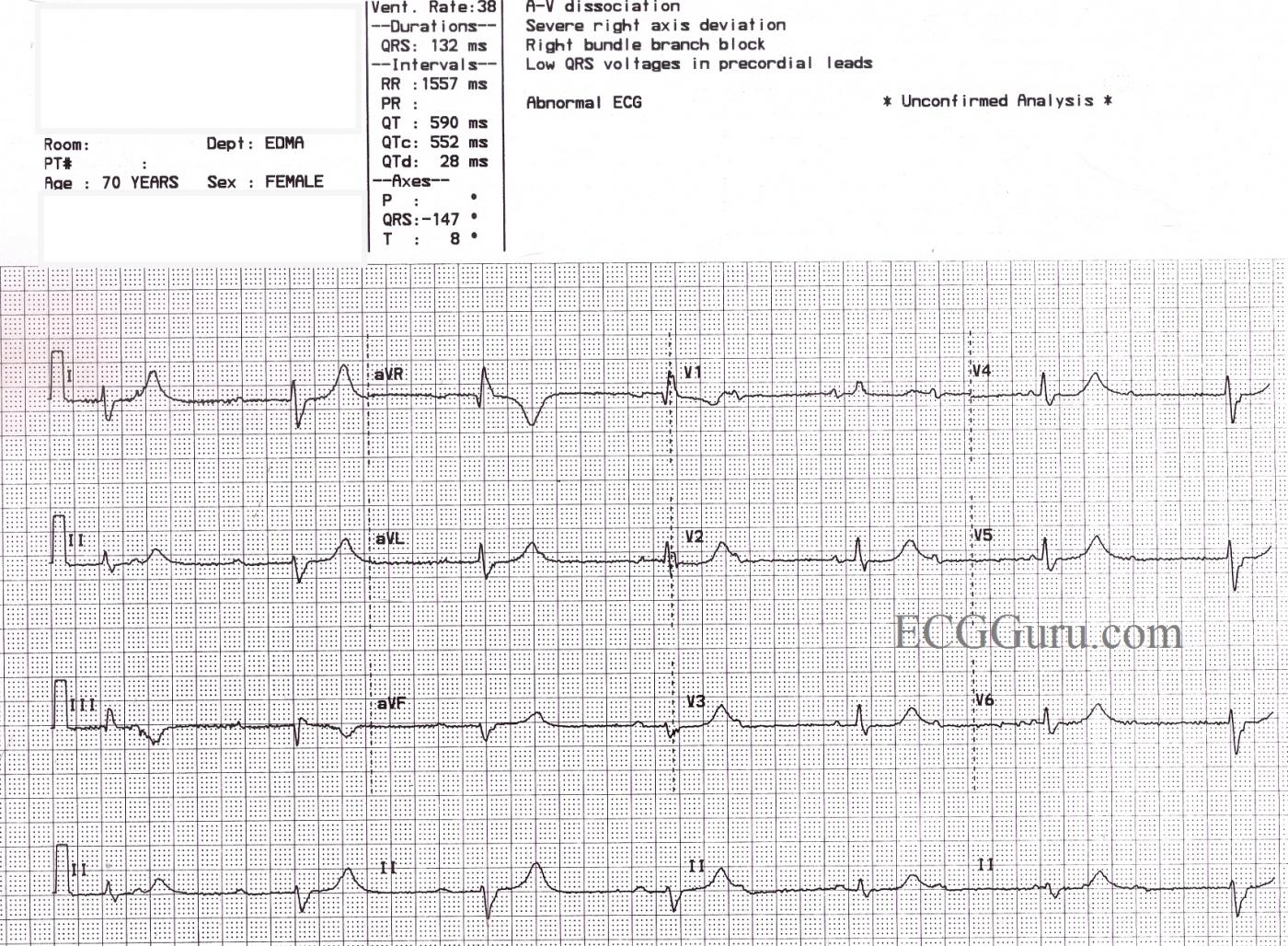
This ECG is from a 70 year old woman for which we have, unfortunately, no clinical information. It shows a sinus rhythm with a rate of about 72 bpm (NSR) with AV dissociation caused by third-degree heart block. The escape rhythm is junctional at a rate of 38 bpm. There appears to be a right bundle branch block, based on the QRS duration of 132 ms, and a wide S wave in Leads I and V6. The precordial leads do not show the usual RBBB pattern of rSR' in V1 and V2, and the r wave progression is poor (non-existent). This is felt to be due to poor lead placement (a good teaching point). Of interest, the ECG machine has reported a "severe right axis deviation" based on the tall upright R wave in aVR and the deep S in avF. In RBBB, the first part of the QRS represents left ventricular depolarization, and the terminal wave represents the delayed right ventricle. In effect, the two ventricles have their own electrical axes, which we can see because the ventricles are not depolarizing simultaneously. The axis of the LV appears to be normal in this tracing.
In addition to the above, this patient has a very prolonged QT interval. The QT is longer in bradycardic rhythms, but when corrected to a standard of 60 bpm (QTc), this patient's QT interval is still prolonged at QTc: 552 ms. Without clinical data, we cannot speculate as to why this patient's QTc is prolonged, but it can be a very dangerous situation. Follow the links for more information on QT prolongation and Torsades de Pointes and Long QT Syndrome.
As always, we welcome comments from our members adding insight to this interesting ECG, and also questions you would like to ask our Guru members.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Probable 3rd Degree with Changing QRS Morphology
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Great comment!
Great thoughts Dr. Grauer. I too was a bit perplexed by that changing QRS morphology - it definitely exceeds what I consider to be WNL for respiratory variation. I'm glad you already covered the possibilities far better than I could have.
Vince D
Vince D
http://www.medialapproach.com
education
Add a comment as donna jackson
Top comments
Stream
donna jackson
1 second agoShared publicly
I found out 2 years ago that I have LongQT. Then genetic test came back I know it's LQTS1 . My ECG showed a long QT for years before that. Most doctors I've seen have no clue what to read and even more concerning don't seem to care enough to study up. Cardiologists even go into a blank stare too. I came to your blog after searching the internet for hours to find my way.Sudden death is not as rare as one is led to believe, so I fail to see why the patient has to be the person fighting their way through the system to avoid the dreaded moment of crisis. Just because it's genetic doesnt mean you ignore it in your training. ( it's often acquired and can be temporary too)There's an ECG machine in modern ambulances and ER and teaching hospital should have an electrophysiologist and he should train the ER nurses to read this. Before anymore patients die while people scratch their heads. Secondly train Aneasthetists so I dont have to beg them to consider my condition while they glaze over. I can only.imagine what families go though who have no insurance. Because genetic testing costs. Since the list of medicines that can cause LongQT leading to Tosades is long and includes every class of drugs. I fail to see how anybody from GPs who prescribe to Emergency medicine isn't trained to at least know the syndrome.Thankyou for the blog