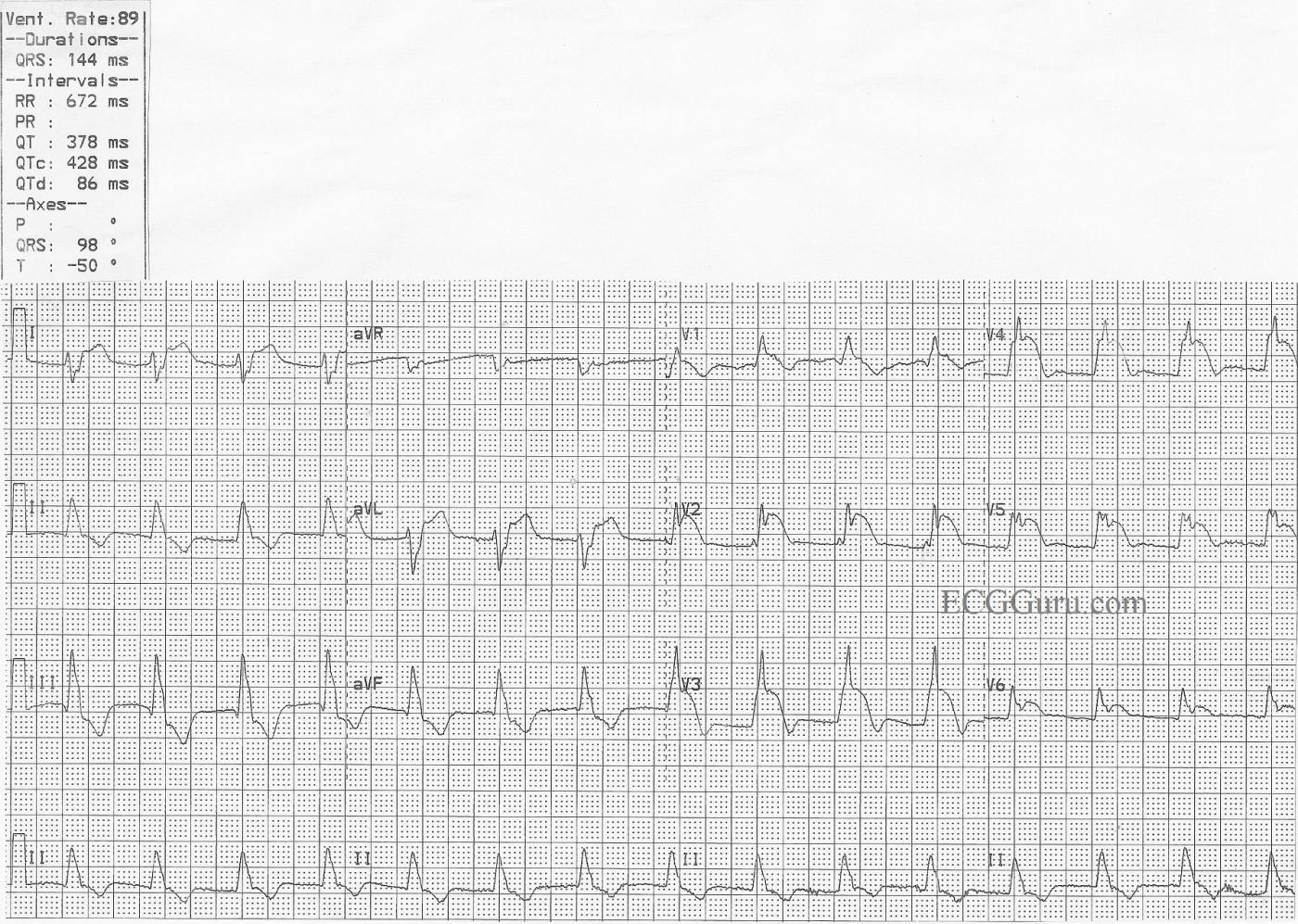
This ECG was obtained from a patient who suffered an occlusion of the left main coronary artery. ST elevation is seen in Leads V1 through V6, as well as I and aVL. This is an indicator that the circumflex artery is included in this M.I., and the occlusion is above the bifurcation of the LM and the circ. The patient also has a right bundle branch block and a left posterior fascicular block. This bi-fascicular block can be a dangerous complication of acute M.I., as two of the three main bundle branches are no longer functional.
The ECG shows typical ST depression, probably reciprocal to the elevation, in the inferior leads.
The right bundle branch block is diagnosed by the following criteria: 1) Wide QRS; 2) Supraventricular rhythm; and 3) rSR' pattern in V1 with Rs with a wide little s wave in Leads I and V6.
The left posterior fascicular block is diagnosed by right axis deviation and by ruling out other causes of right axis deviation. In RAD, Lead III will have a taller positive ( R ) wave than Lead II, and a negative Lead I.
This type of occlusion is often called the "Widow Maker", and requires very rapid intervention to restore blood flow and prevent complicatons. If there is good news, it is that there are no pathological Q waves, which would indicate necrosis, and this patient was taken quickly to a full-service cardiac center with interventional cath labs and open heart surgery available.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Acute Left Main Occlusion - with RBBB/LPHB
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Location of lesion
Agree with Ken about location of lesion. I don't believe I ever saw the cath on this patient, but is was reported to me as a "left main" occlusion. I'm not sure if he fell short of being 100%, but I suspect the lesion was near the bifurcation of the circ. The patient was treated in a full-service cardiac center, but we do not have a record of the outcome.
Dawn Altman, Admin
poor collateralisation?
I’ve been reading a Spanish study (authors include Bayes de Luna) that was published in J Electrocardiol in 2012. This was of a series of 7 patients who had acute LMCA occlusion that presented with an ECG showing ST elevation typical of anterior MI. 4/7 patients died, and the authors hypothesised that this pattern indicated a lack of collateral circulation and conferred a grave prognosis. Most of their patients presented in shock; 4/7 had RBBB and all had left anterior fascicular block. It was stated that the ‘typical’ LMCA occlusion ECG pattern of widespread ST depression + ST elevation in aVR and V1 is due to widespread ischaemia when there is a well-developed (but still inadequate) collateral circulation.
If, therefore, acute LMCA occlusion with ST elevation indicates poor collateralisation and consequently a very poor early prognosis, this may be why it is seen infrequently. Perhaps the ‘typical’ pattern with ST elevation only in aVR and V1 is only seen much more frequently because the patients, having a good collateral circulation, tend to have a better survival rate.
Ken -minor point, but should we say that the left poster hemifascicle is perfused rather than innervated by the coronary arteries? (sorry, I know that everyone hates a pedant).
Dave R
Thanks, Dave - Very Interesting
I do not believe I have cath images from this patient - it was from a huge file of ECGs with only small, hand-written notes on them. (sigh...) Your comment has made me REALLY want to see the cath images, and I will be scurrying back to my voluminous files to see if I can find a cath that goes with this ECG. That will require that I find the original ECG without the patient info redacted. I sure do wish I had kept better records all those years - but I was busy working, and didn't have the luxury of time, taking care of multiple high-risk patients undergoing procedures. Because most of my ECGs come from donations from friends, my 30+ years in the ED, and several years in the Cardiac Center Admit and Recovery Unit (Cath lab, EP lab, Procedures,), I was usually too busy to do more than take a quick copy and scribble a note.
Would welcome comments from cath lab people on what you have seen regarding left main and proximal LCA occlusions.
Dawn Altman, Admin