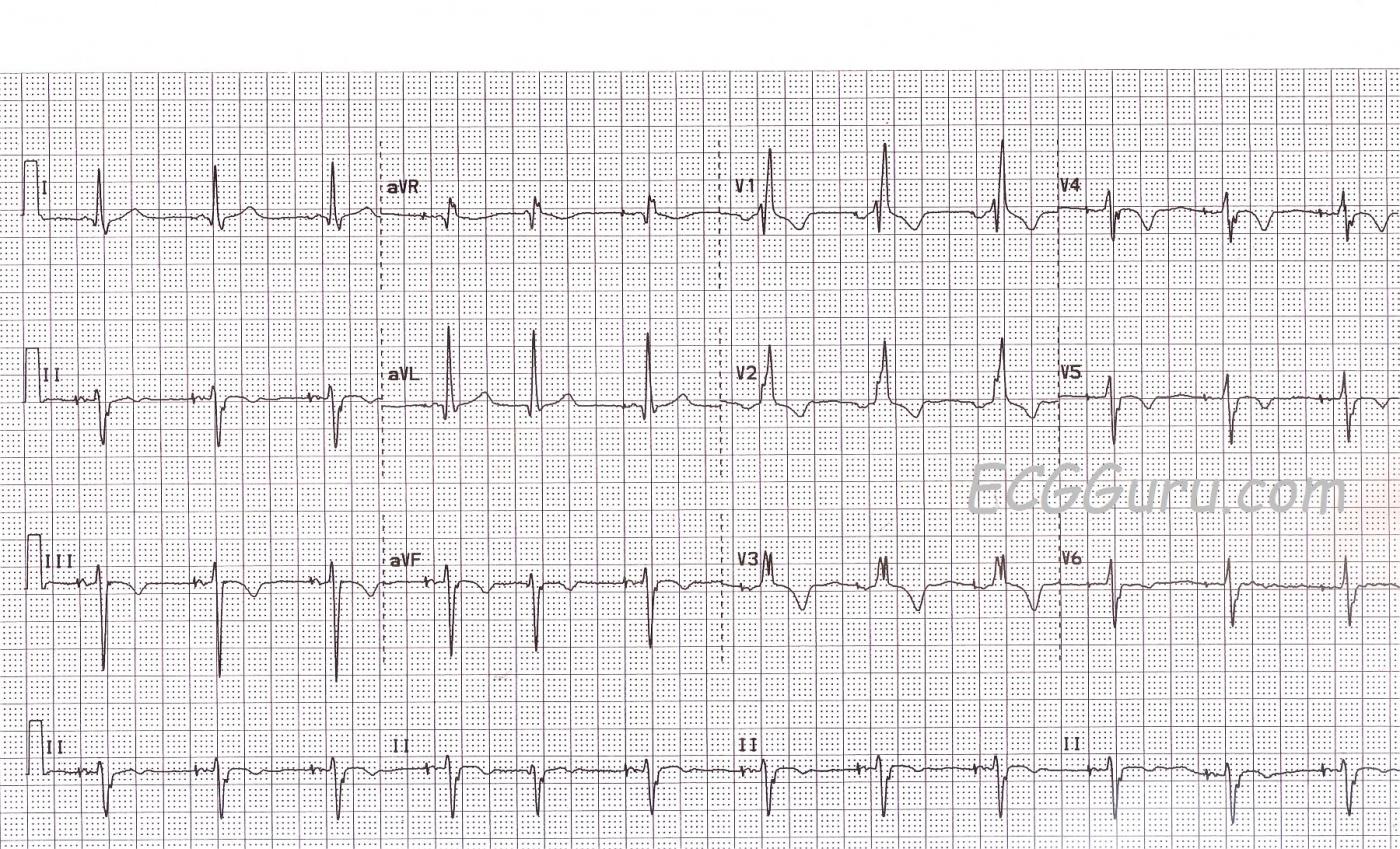
No instructor's collection should be without an atrial paced rhythm OR a right bundle branch block. Here, you get both. First, the atrial pacing. This patient had a sinus node problem, but his AV conduction system was functional (if not perfect). At this time, he is able to conduct impulses from the atria to the ventricles. What he cannot do is reliably produce the impulse in his atria. So, this pacemaker is currently pacing the right atrium, producing a paced "P" wave, which is then conducted to the ventricles. The fifth beat on the strip shows a "native" beat - one produced by the patient. No P wave is seen, so it is presumed to be a junctional beat.
As for conduction through the ventricles, there is a right bundle branch block. The left bundle branch is ensuring that the ventricles receive the depolarization "message", and the ventricles are depolarizing and contracting. However, the right ventricle gets the message a little late, since is arrives from the left ventricle, and not through a functioning right bundle branch. This produces a terminal wave on each QRS that represents this delayed depolarization of the right ventricle. In leads oriented to the left side of the heart, like I and V6, it is seen as a wide little S wave. In V1, which is oriented to the patient's right, we see an R prime (R'), producing the easily-recognizable rSR' pattern of RBBB.
For your more advanced students, this patient has atypical T waves for RBBB. Normally, the T waves axes should be OPPOSITE that of the terminal portion of the QRS. So, Lead V1 correctly shows an inverted T wave, since the R' is a positive deflection. There are inverted T waves in Leads III, aVF (II is biphasic), as well as in V4, V5, and V6. We expected upright T waves here. Because we do not have clinical information for this patient, we will call them "non-specific" T wave changes, remembering that inverted T waves can be a sign of ischemia.
ALSO: As noted in Dave Richley's comment below, there is a left axis deviation, with a negative Leads II, aVF and III, and a positive I and aVL. This indicates left anterior fascicular block, which is rather common with RBBB, since the right bundle branch and the left anterior fascicle share a blood supply. So, this person as a "bi-fascicular block".
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
left axis deviation
It's probably worth pointing out that in addition to what Dawn describes there is also a big left axis deviation typical of left anterior fascicular block.
Dave R
Thanks, Dave
Yes, I omitted that accidentally, as it is rather glaring. I will add an addendum. Thanks so much.
Dawn Altman, Admin
Atrial Pacing and a LOT MORE Going On (RBBB,LAHB,T waves)
As described - this tracing shows atrial pacing. But ventricular complexes are not paced - so we can fully analyze them for QRS and ST-T wave morphology.
Ken Grauer, MD www.kg-ekgpress.com [email protected]