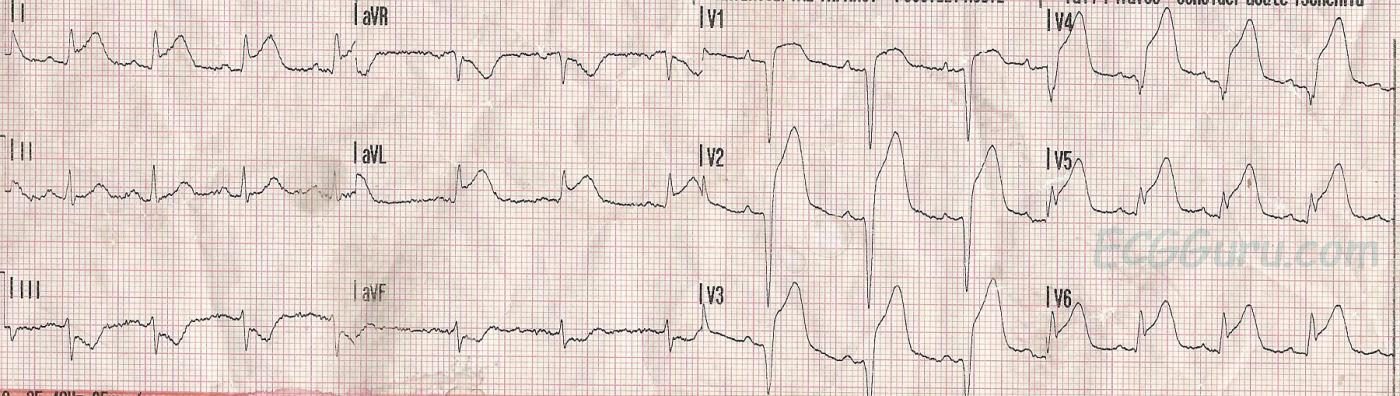
This week's ECG is from a 47-year-old man who experienced a sudden onset of chest pain while mowing his lawn. He went on to suffer a cardiac arrest and was resuscitated. We do not have long-term followup on his outcome.
The experienced person will have no difficulty identifying a large acute antero-lateral wall M.I. There are massive ST segment elevations in Leads V1 through V6, reflecting acute injury from the septal side of the anterior wall (patient's right) to the anterior-lateral wall (patient's left). There are also ST elevations in Leads I and aVL, reflecting the high lateral wall. This indicates, and was confirmed in the cath lab, that the lesion is proximal - at or above the bifurcation of the left anterior descending artery and the circumflex artery. The ST depressions in the inferior wall leads (II, III, and aVF) likely represent reciprocal changes. You will note that the ST depression in Lead III has a very similar shape to the ST elevation in Lead aVL.
More bad news for this patient is the presence of pathological Q waves in Leads V1 through V4, reflecting transmural death of the myocardial tissue. This causes akinesis and poor left ventricular function. In addition, it's not only muscle tissue that dies, but also electrical structures , such as bundle branches. Papillary muscles can be infarcted, causing valve malfunction. And remember, all patients who have ST elevation due to acute injury are vulnerable to ventricular tachycardia and ventricular fibrillation, due to re-entry mechanisms in injured tissue.
This ECG will allow instructors to discuss with their students:
* which leads reflect changes from which parts of the heart
* what the ECG signs of acute M.I. are
* the pathophysiology of pathological Q waves
* the effect of damage to various parts of the heart on the patient's condition and symptoms
This "classic" M.I. pattern should be taught to all health care professionals who work in settings where ECG is used.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
PEARLS in Assessment of the "Culprit Artery" with Anterior STEMI
PEARL: Distinction between left-main disease vs proximal LAD occlusion may be suggested on ECG by the relative amount of ST elevation seen in lead aVR compared to lead V1.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Off topic
Ken, on the topic of Bayes de Luna (who I'm just starting to appreciate as one of the true rock stars of electrocardiography), have you read his book "The 12 Lead ECG in ST Elevation Myocardial Infarction"? I recently got my hands on a pdf and I wish I had found it a couple of years ago. It pretty much clarifies all of the concepts regarding localizing culprit lesions that I've slowly accrued through experience and guess-and-check over the past two years in 50-some pages. I kept thinking, "I wish someone would write a book where they just describe patterns of ST-elevation and injury vectors and correlate them with coronary anatomy and pathology." Turns out he did and I just didn't know it.
Vince D
http://www.medialapproach.com
Correction
Just to clairfy, in the discussion you state, "the lesion is proximal - at or above the bifurcation of the left anterior descending artery and the circumflex artery." What you mean to say is that it is at or above the takeoff of the first-diagonal and first-septal arteries. If it was proximal to the LCx then we'd be talking about a left-main lesion.
Vince D
http://www.medialapproach.com