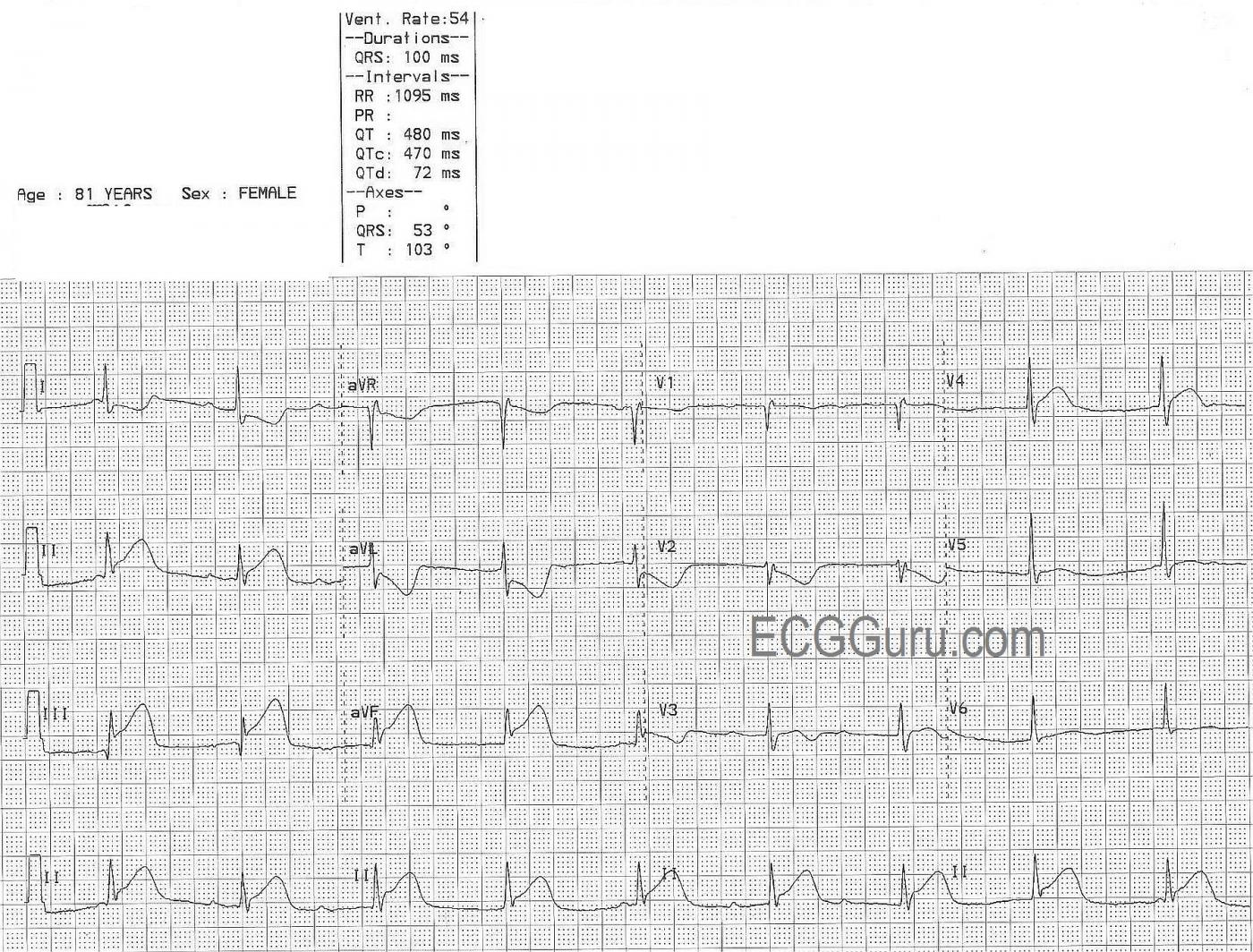
This ECG is from an 81 year old woman with an extensive history of coronary artery disease. She was experiencing chest pain at the time of the ECG. We can clearly see ST elevation in Leads II, III, and aVF, indicating an inferior wall ST-elevation M.I. (STEMI). There are reciprocal ST depressions in Leads I and aVL. There are subtle and less specific ST changes in V1 (flat ST and T), V2 (ST depression), V3 (ST elevation and inverted T wave), and V4 through V6 (slight ST elevation). The flat, horizontal shape of most of the ST segments is another clue to her CAD. What coronary artery do you think is the culprit for the ST elevation?
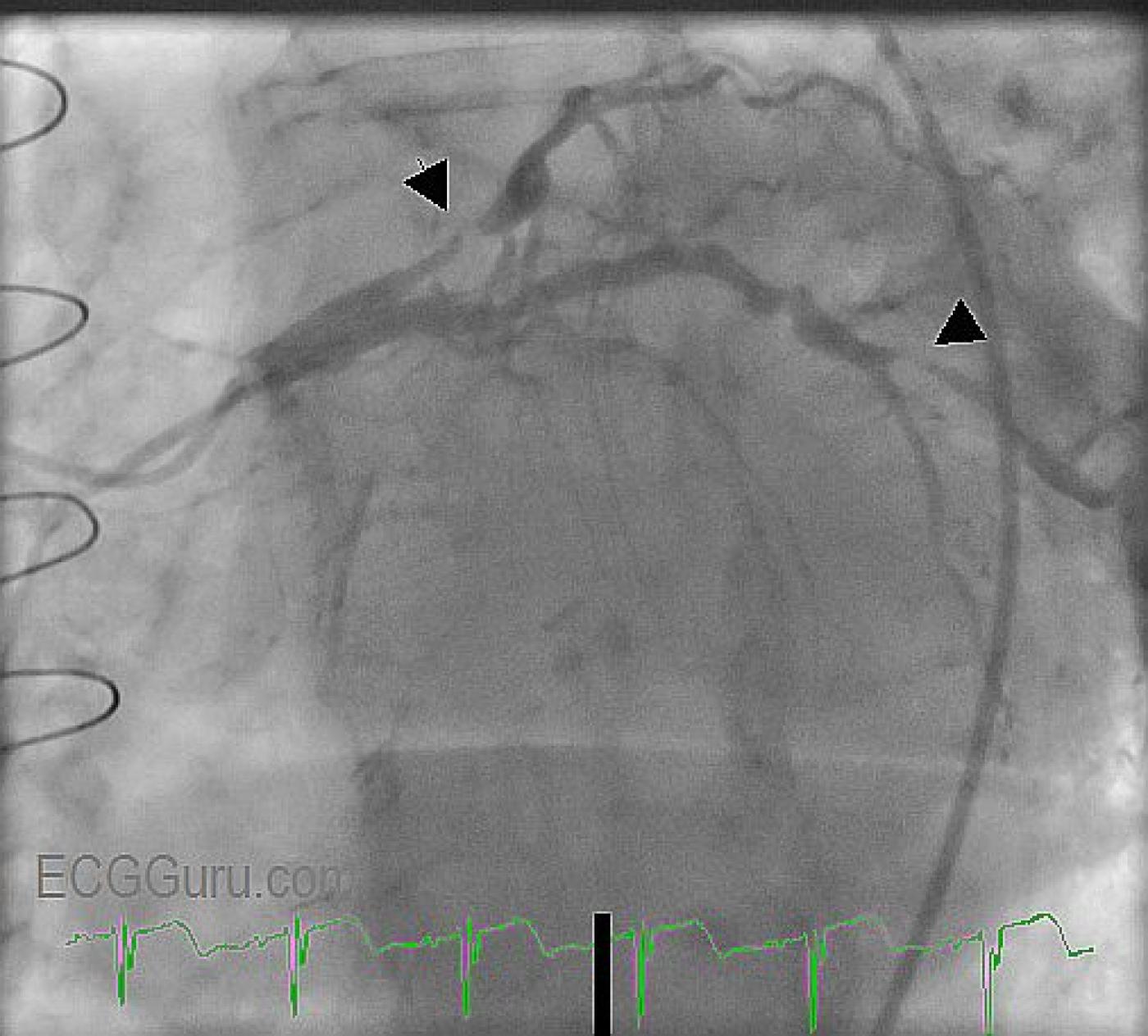
This patient received coronary angiography, so we do not have to guess at where her lesions are. She was found to have an occluded left internal mammary artery (LIMA) graft.
The left anterior descending coronary artery (top of view) is very diseased, with some extremely narrow areas. The circumflex artery is large and covers a lot of area, but it, too, is very diseased, with a critical occlusion (marked with arrow). On this day, the circumflex artery received angioplasty and stents. The patient's right coronary artery was patent.
In approximately 85% of the population, the RCA supplies the inferior wall of the heart. In most of the rest, a branch of the circumflex supplies the posterior/inferior wall.
This patient also has a very interesting arrhythmia. We see P waves (numbered) that appear regular for three beats, then we see no P waves for a pause. Then, three more P waves appear. There is no readily-seen "hidden" P wave in the ST segments or T waves. Even though there appear to be "progressively prolonging PR intervals", the PR intervals of each group of three do not match the other group of three. The first "PRI" - P wave number 1- and the last one - P wave number 7 - appear too short to be normal PR intervals. The ventricular rate is regular, and the QRS complexes are slightly wide at .10 sec. The rate is 54 bpm. This suggests junctional rhythm.
We are eager to hear your comments regarding this rhythm.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Acute STEMI- Which Vessel? - What Rhythm?
VERY interesting case by Dawn - both for the rhythm as well as the 12-lead ECG. It is always insightful when we have "the answer" (= cath films) - since we can then KNOW where the lesion is. As always - I do my best NOT to bias my interpretations - so I had no idea of what the cath showed until AFTER I interpreted the tracings. One learns more this way.
Ken Grauer, MD www.kg-ekgpress.com [email protected]