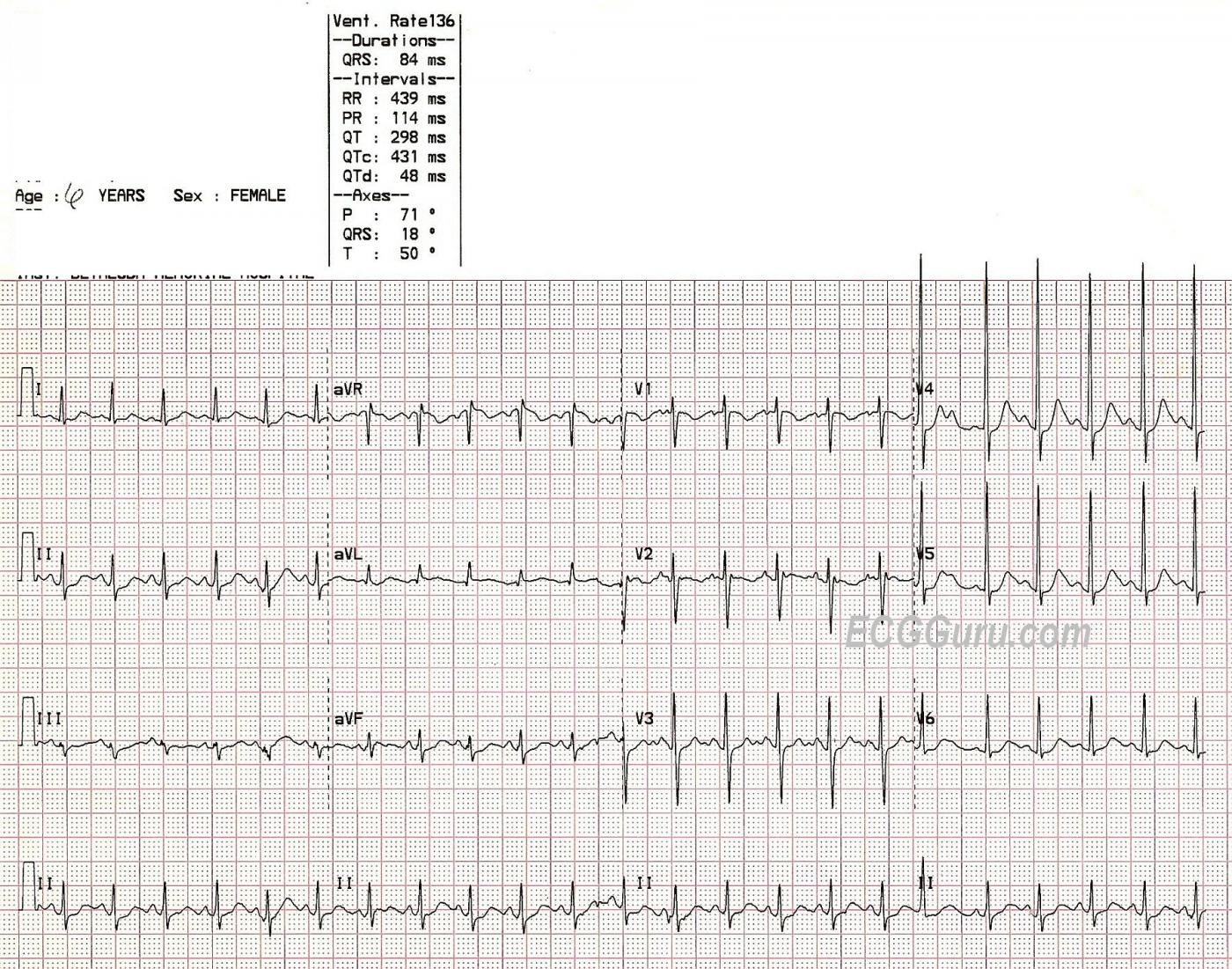
A six-year-old girl was found with her two younger siblings and her mother, unconscious, in a room filled with carbon monoxide. The mother had been using a charcoal grill inside the house. She managed to call 911 before losing consciousness, and the fire rescue paramedics broke into their house, saving them. This six-year-old required treatment in the pediatric intensive care unit, but recovered completely. The lesson for our students is to judge rate in the setting in which it is found. The heart rate here is 136/min. Normal for a child of six is usually between 80 and 100 at rest. This child is severely hypoxic, and she has sinus tachycardia. It would be a mistake to assume her rate is normal because "all children have fast heart rates". Also, children with sinus tachycardia can be so fast, they appear to have PSVT. The onset and offset can be excellent clues to the origin of the rhythm. Sinus rhythms can be expected to speed up and slow down gradually, unlike PSVTs, which have sudden onset and offset. The most important consideration is that sinus tachycardia usually has an APPARENT CAUSE: exercise, anxiety, hypoxia, hypovolemia, fear ,,,, the list is a long one. Once it is determined that the patient has sinus tachycardia, efforts usually focus on the elimation of the cause.
We welcome any comments on this ECG, perhaps taking the discussion to a more advanced level.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
T Waves
CO high incidents of MI, T wave abnormal V1V2, lead III T Wave???
TWI is normal in V1. As is
TWI is normal in V1. As is inverted P waves.
A very lucky
A very lucky family, to say the least. I'd be interested in seeing a post recovery ECG. No doubting this is a sinus tachy, but there are some curious changes which certainly would have had me worried when the ECG was taken. Starting with the QT interval - it appears prolonged, at greater than half the R-R interval, or am I seeing a U wave embedded in it? Secondly, some ST depression in the inferior and anterolateral leads - II, aVF, V3-V6, and there also appears to be a smidgen of ST elevation in aVR. I also note what appears to be either a PAC or junctional escape beat (18th QRS on the rhythm strip). Electrical criteria for LVH is also present. Certainly many of these changes can be attributed to hypoxia and CO poisoning, but I'd be interested to hear what others think about the QT and high voltage in V4-V5. Paed. ECG's are by no means my forte, so look forward to hearing from others.
Re the QT - the Rate is Too Fast to Tell ....
Hello benant2. I am sorry for my delay in responding to your question about the QT interval - but I am somehow just seeing it now. The heart rate of this child is simply too fast to allow us to say much about the QT interval. The "not more than half the R-R interval" is a rule of thumb that works best at rates <90/minute - and does not do well at all beyond 110/minute ... QT prolongation would seem low on the list of concerns about this unfortunate child - but given the marked tachycardia - we really can't comment on the QT in any meaningful way.
You may be interested in my brief on-line review of this topic - GO TO: https://www.kg-ekgpress.com/ecg_web_brain_DEMO_-_chapter_7_-_qt_interval/
Hope that answers your question.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
I have a LOT to Discuss about this simple Sinus Tachycardia!
Dawn's tracing for this week simply shows Sinus Tachycardia @ 135/minute in a 6 year old child. That said - IF you were teaching a group of intermediate (or even advanced) providers — there IS a lot you could talk about regarding this tracing.
Ken Grauer, MD www.kg-ekgpress.com [email protected]