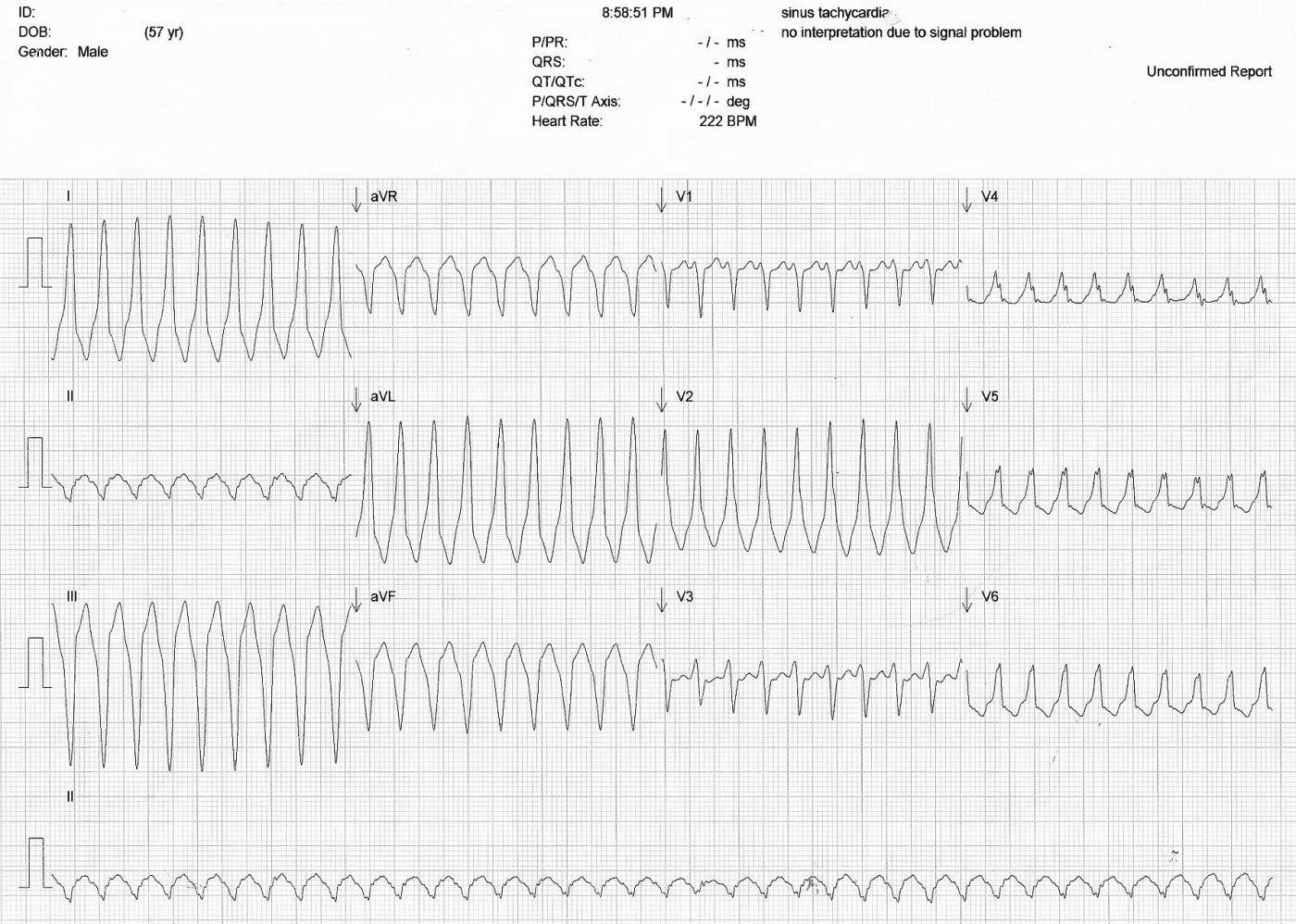
This ECG was submitted by Sebastian Garay, EMT-P and ECG Guru (and ECG Guru Member sebmedic). It is a very interesting case of wide complex tachycardia in a patient with Wolff-Parkinson-White.
This is from a 57 year old man who sought medical help for a complaint of palpitations. He was known to have WPW. The paramedics determined that he was hemodynamically unstable, and in light of the wide-complex tachycardia, they performed a synchronized cardioversion at 100 j. The patient converted to the rhythm shown in the next ECG. The paramedics then administered a Lidocaine bolus and drip, considering this to be a ventricular tachycardia. The patient arrived in the Emergency Dept in improved hemodynamic condition.
This ECG can be used to teach V Tach for beginner students, WPW and WCT tachycardia differential diagnosis for more advanced students. It is also a good ECG for axis discussion, and for how lead placement affects the final product.
The differential diagnosis here is 1) V Tach and 2) SVT with aberrant conduction or left ventricular conduction delay. For a discussion of ECG criteria which help us diagnose WCT, see the "Ask The Expert" column from Jan. 11, 2012. Characteristics that make this look like V Tach include: wide complex and significant left axis deviation. Features which may favor a diagnosis of SVT are the pre-existing WPW and a rate of 222/min. There are no p waves seen. NOTE: V2 in this ECG appears to reflect electrode mis-placement, as it does not "make sense" in the normal progression of the QRS complexes in the precordial leads. It is clearly "out of place".
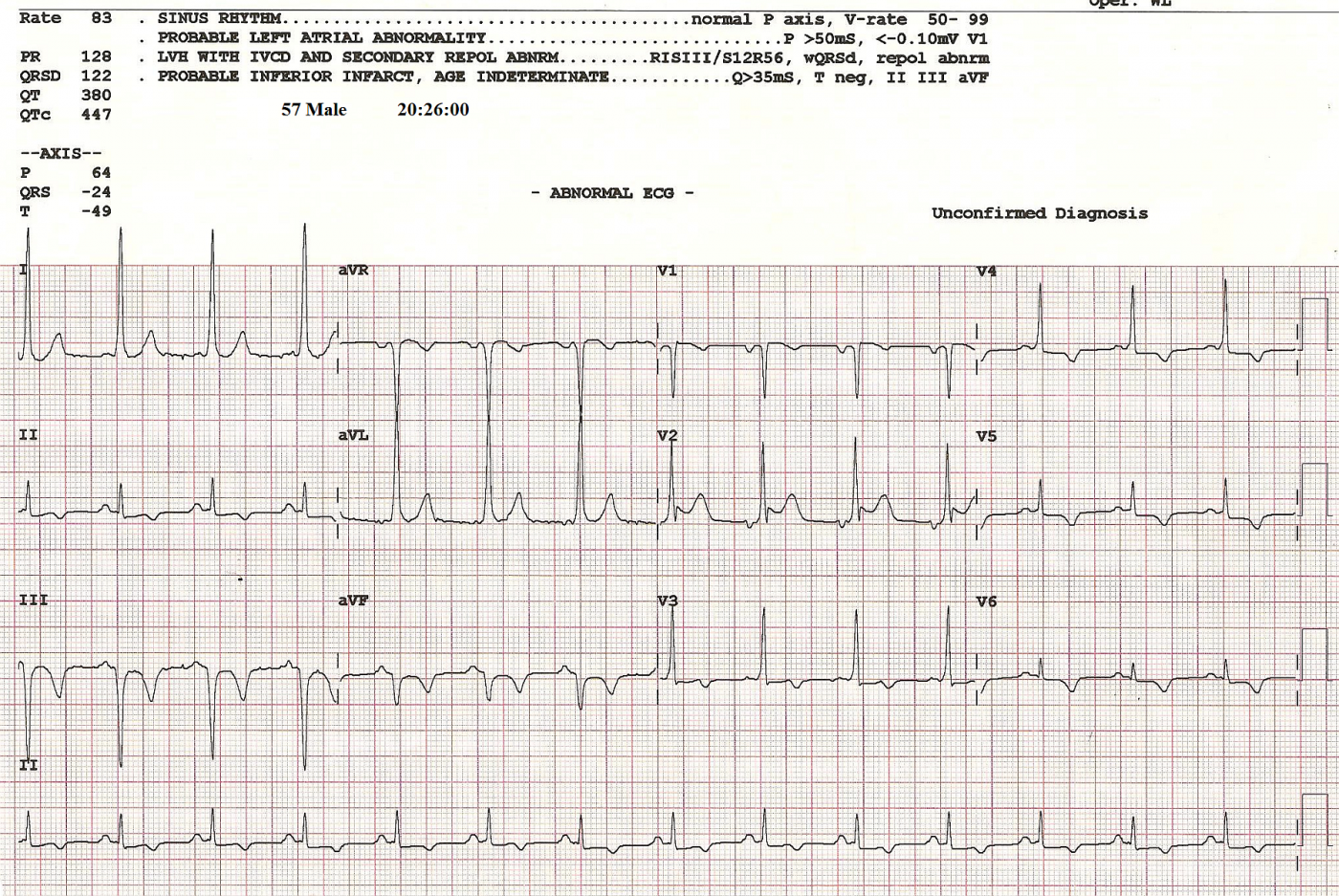
The second ECG shows the same patient after conversion of the tachycardia. The delta waves of WPW are easily seen.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Exerpt from Sebastian Garay's notes accompanying these ECGs
The initial ECG from the urgent care shows a very fast rate and what appears to be a wide QRS. Further inspection of leads V1 and V3 show what seems like a discernible p wave in conjunction with the QRS. This would rule out that the rhythm was ventricular in nature. I did some research and determined that the reason why the QRS is wide is due to the conduction being AV re-entrant and the ventricles are being activated through the accessory pathway. It is also antidromic due to retrograde conduction going back to the atria through the AV junction.
The followup ECG after the pt converted shows a typical WPW pattern with delta waves visible in lead V2. Very fascinating.
Dawn Altman, Admin
From Jason Roediger, via email:
One thing I immediately noticed about the ECG of the wide QRS complex tachycardia is that something doesn't look quite right about the transition in the precordial leads. Lead V1 shows a diphasic rS complex that is predominantly negative. V2 is a large monophasic R-wave that is wholly positive. V3 is now back again to a diphasic rS complex. (S.G.) even makes a point of jumping over lead V2 in order to draw attention to what they think is a P-wave in only those two particular leads. It stands to reason that if a P-wave is going be visible in both V1 and V3, then is should be equally visible in V2 as well (maybe even more so). Lead V4-6 are all back to being predominantly positive again. This "staggered" look and lack of normal QRS transition seems out-of-place and not at all natural to my eye. I think that in the heat of the moment, someone attached a precordial cable (or two) to the wrong electrode. I'm not convinced there are any visible P-waves or other atrial activity here. As it is, I don't think there's any way to completely rule out the possibility of this being monomorphic ventricular tachycardia.
I do however agree with the interpretation of W-P-W on the ECG displaying sinus rhythm and I think the wide QRS complex tachycardia is probably some form of preexcited tachycardia (probably antidromic tachycardia over a right-sided accessory pathway assuming, of course, that V1 is correctly attached to the right electrode).
It's kind of scary how the computer says there is a signal problem when the ECG is of high quality and free of artifact. Furthermore, why would the computer consider this to be sinus tachycardia at a rate of 222/min???
Dawn Altman, Admin
Excerpt from Dr. Ken Grauer, MD, email:
My first thought on looking at the WCT tracing was that it looked like WPW with flutter EXCEPT that the rate (~ 220/minute) is clearly slower than the ~300/minute expected with flutter. Therefore - IF this was the ONLY tracing you had - VT should clearly be assumed until proven otherwise. That said - (S.G.) gave us the history that the patient has known WPW - and this is confirmed in the post-conversion tracing. In view of this - I feel this tracing is much less likely to represent VT.
Dawn Altman, Admin