Comprehensive list of criteria
PermalinkSubmitted by jer5150 on Tue, 01/10/2012 - 22:17
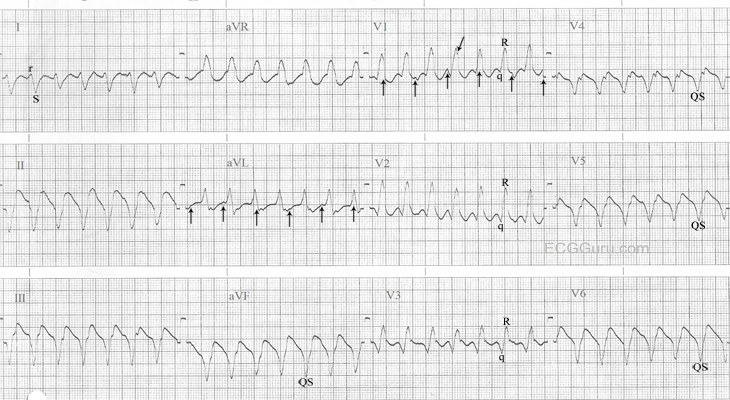
INTERPRETATION: Ventricular tachycardia (rate about 163/min) presumably originating from the left ventricle (LV).
Overwhelming evidence that this is ventricular tachycardia are as follows:
1.) The ventricular tachycardia is apparently dissociated from a sinus tachycardia at a somewhat slower rate of about 123/min (best seen in leads V1 and aVL; vertical arrows). While not nearly as clinically significant as those types of double tachycardia caused by digitalis intoxication, this example might technically qualify as a form of “double tachycardia” since both the upper and lower chambers of the heart are exceeding a rate of 100/min.
2.) The duration of the QRS interval is so-called “wide-wide” (i.e., > 0.14s) at about 0.19s to 0.20s.
3.) The predominantly negative rS complex in Lead I and wholly negative QS complex in aVF indicate an axis of roughly about -120 and would place it in the right upper quadrant (i.e., “No-Man’s-Land” or “N-M-L”). This is suggestive of an apical origin of the tachycardia.
4.) Brugada criterion # 1: There are no RS complexes in any of the V leads (here they’re either qR or QS complexes.) Brugada pointed out that if none of the V leads contained a diphasic RS complex, then there was no need for any further analysis, the tachycardia was unequivocally ventricular in origin. 2
5.) The presence of a monophasic QS complex in V6 is more diagnostic of ventricular tachycardia than just a rS complex; especially if associated with a QRS complex in V1 that is predominantly positive. By Dr. Marriott’s estimation, this combination only occurs in about 20% of all left ventricular tachycardias (LVT).
6.) Cogent evidence arguing against this being the result of conduction over an accessory pathway are threefold:
a. The wholly negative QS complexes from V4-6 are also suggestive of an apical origin of the tachycardia. Since all accessory pathways enter the ventricles at their base, accessory pathway conduction is effectively excluded; and . . . 1
b. . . . a qR complex in any of the five leads, V2-6 (here in V2-3) also excludes preexcited (W-P-W) tachycardia; and . . . 1
c. . . . the presence of more QRS complexes than P-waves (because in any form of preexcited tachycardia, the atria are involved in every beat). 1
7.) The QRS complex in V1 is not a monophasic R-wave. Rather it is a diphasic qR complex with very subtle notching / slurring on the downstroke (oblique arrow) of the R-wave (i.e., so-called taller left “rabbit-ear” equivalent.)
8.) The q-waves in V1-3 are superficially mimicking the negative component (i.e., nadir) of an atrial flutter wave but right-sided chest leads do not usually show the typical “saw-tooth” pattern so often seen in inferior leads II, III, and aVF. Atrial flutter waves in V1 usually take on the appearance of little positive “P-like” waves. What looks like a retrograde atrial impulse immediately following a QRS complex in V4 is actually part of the QRS complex itself.
References / Sources.
1.) Marriott, HJL. Emergency Electrocardiography. Naples, Fl.: Trinity Press, 1997, p. 60 - 71.
2.) Nelson's EKG Site: http://nelsonsekgsite.com/
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Criteria for VT
GREAT post by Jason - showing why with 1,000% certainty this tracing is VT!
Ken Grauer, MD www.kg-ekgpress.com [email protected]