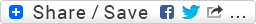
Patient's clinical data: This 12-lead ECG is from an adult patient of unknown age and gender (at the time of posting). Active medications included Atenolol. Patient's only complaints and symptoms were cramps and palpitations in the form of "an occasional extra beat". This ECG was the patient's initial "baseline". Based on what the patient's primary care provider (PCP) misinterpreted in this ECG, the patient ended up having an erroneous diagnosis listed among their "active problems". Their computerized medical record that was never expunged of this bogus information. A cardiac electrophysiologist was consulted and subsequently refuted the PCP's interpretation.
Questions:
1. What might the patient's PCP misinterpreted this as?
2. What is the actual interpretation?
3. Is there any form or manifestation of AV block here? If so, what is it?
4. What is the primary disturbance of rhythm here? What is a secondary finding to that primary disturbance?
http://www.amjmed.com/article/0002-9343%2858%2990309-7/abstract
-
- jer5150's blog
- Log in or register to post comments
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
I think more strips would
I think more strips would show this better. Off this 12 lead, I suspect that the atrial rate is about twice that of the ventricular rate. (looking at v6 shows what I suspect might be a p wave the best). *about* twice being the operative word. The p-p interval is consistant, and the r-r interval is consistant, but they are not the same consistancy. The ventricular rate is slightly faster than twice that of the atrial rate. So I'd say this is a 3rd degree heart block with the ventricles being paced at or near the av junction, possibly brought on by the beta blocker. What the patient was initially diagnosed with based off this 12 lead I can't guess, as all of the things I could think would contra-indicate a beta blocker. I suspect there also may be a K+ defficiency given the cramps and the diffuse t waves.
So the fact that I can't come up with another interpretation, leaves me with the unfortunate thought that my diagnosis is in all likelyhood the same as the PCP . :P
Probably U-waves
I think those positive deflections best seen in V6 are likely to be U-waves associated with the bradycardia. The amplitude of the P-waves in other leads shows that there would have to be a much larger deflection for those to be actually P-waves.
Additionally, if they were P-waves, they exist at <1/2 P-P interval and have a different morphology of the ones you can see so they would be PAC's. This would indicate non-conducted PACs as the origin of this patient's bradycardia.
That being said, the PRi progressively decreases in the P-waves we can see leading us to make the determination as to whether they are dissociated or blocked as the two rates are now roughly the same.
Both the P-P and R-R are roughly at 45 bpm, and given that they don't appear to have a clear "block" I would put AV Dissociation on the list higher than Complete Heart Block. But I agree, a longer strip would better elucidate the relationship.
Christopher
sixlettervariable.blogspot.com
ems12lead.com
AV dissociation VS Complete heart block?
Impression: Isorhythmic AV dissociation where atrial and ventricular activity are independent of each other. A junctional escape rhythm at a rate of 42 seems to have taken over the pace making role. Isorhythmic because atrial and ventricular rate are similar. P waves seem to be approaching then moving away from the QRS appearing to be flirting with the QRS complexes.
although third degree AV block is a good differential, I still could not appreciate a beat(P wave) where given ample a opportunity still unable to conduct itself. 1st beat appeared to have a normal PRi, I wonder whether it is conducted or not, I cannot be sure.
Hence top of my list is isorhythmic AV dissociation by default due to underlying sinus bradycardia( culprit could be the atenolol), followed by CHB
Isorhythmic AV dissociation with/without CHB
My impression of this ECG is Sinus bradycardia with Isorhythmic AV dissociation with or without CHB (can't tell)
Initially P waves that precedes QRS complexes may seem like giving rise to ventricular depolarization. But on closer inspection, a few of PR intervals are way too short to be possible to conduct. Therefore the likely reasoning is that atrial and and ventricular activites are running independently at the same pace (isorhythmic).
The initial mis-interpretation that I could think about is ventricular pre-excitation due to the short PR interval eg WPW, LGL syndromes.
AV Dissociation by Default - NO Evidence of AV Block
The underlying rhythm is sinus bradycardia - most likely secondary to Atenolol. The PR interval is too short to conduct for most beats on this tracing! In fact - for all we know NONE of the beats on this tracing are conducting !!! I say this because the R-R interval remains constant - and usually when there is AV dissociation by default (the presumed mechanism here) - there will be a slight-but-measurable change in R-R interval, and I'm not sure that we are seeing that here ... The PR preceding beats #1 and #5 might be conducting - but really we NEED additional rhythm strips to know for sure what the PR interval that will conduct is .... (perhaps there is underlying 1st degree AV block and none of the P waves here are conducting .... ). We just need to see more than one beat in-a-row that may be conducting ...
GREAT case Jason. I know you'll have an insightful laddergram of this I'm hoping you ALSO have some additional rhythm strips that prove whether there is or is not ANY conduction at all on this tracing. THANKS for posting!
Ken Grauer, MD www.kg-ekgpress.com [email protected]
"AV Junctional rythm only"
Heart rate around 45 beats/minutes, P-P and R-R interval constant, No signs of AV dissociation present. Patient was on atenolol, So he/she may have sinus bradycardia thats why the AV junction started firing independently.
The PCP may have interpreted as AV Dissociation(3rd degree heart block).
INTERPRETATION
INTERPRETATION:
1. Slightly irregular sinus bradycardia (rate = 44-47/min) with resulting . . .
2. . . . idiojunctional escape rhythm at a similar rate of 45/min producing . . .
3. . . . isorhythmic A-V dissociation (see laddergram).
4. ST-T changes suggestive of hypokalemia.
COMMENTS:
In a couple of his textbooks, Dr. Marriott simply defined Isorhythmic A-V dissociation as the following: "A-V dissociation with atria and ventricles beating at the same or almost the same rate." I maintain that A-V dissociation (Isorhythmic or otherwise) is never restricted to any specific atrial or ventricular rates. It can occur between any atrial rhythm (e.g., sinus, ectopic atrial, etc.) and any ventricular rhythm (e.g., junctional, ectopic ventricular, ventricular paced, etc.). The sole requirement for A-V dissociation is that the atrial and the ventricles are beating independently. If the respective rates of both the atria and ventricles are identical or similar, and yet they remain dissociated, then the A-V dissociation qualifies as being "Isorhythmic". The ECG above should not be confused with Complete A-V block. Here, the primary disturbance of rhythm is a marked sinus bradycardia which is the result of the patient's Atenolol. Both the A-V dissociation and the idiojunctional escape rhythm are secondary to the sinus bradycardia. Inexplicably, the patient's PCP grossly confused and misinterpreted this ECG as Wolff-Parkinson-White (W-P-W) syndrome. When I saw W-P-W listed among the patient's active problems, I asked him if he had W-P-W to which he denied ever hearing of that diagnosis. He did not strike me as a "poor historian", so I reviewed his serial ECGs and found out that his very first "baseline" ECG was misread as W-P-W and was never corrected in the patient's record.
In several of the precordial leads, there is a subtle "roller coaster effect" between the negative T-wave and the positive U-wave which is superficially mimicking a prolonged QT interval. At the time this ECG was recorded, the patient was hypokalemic at 3.2.
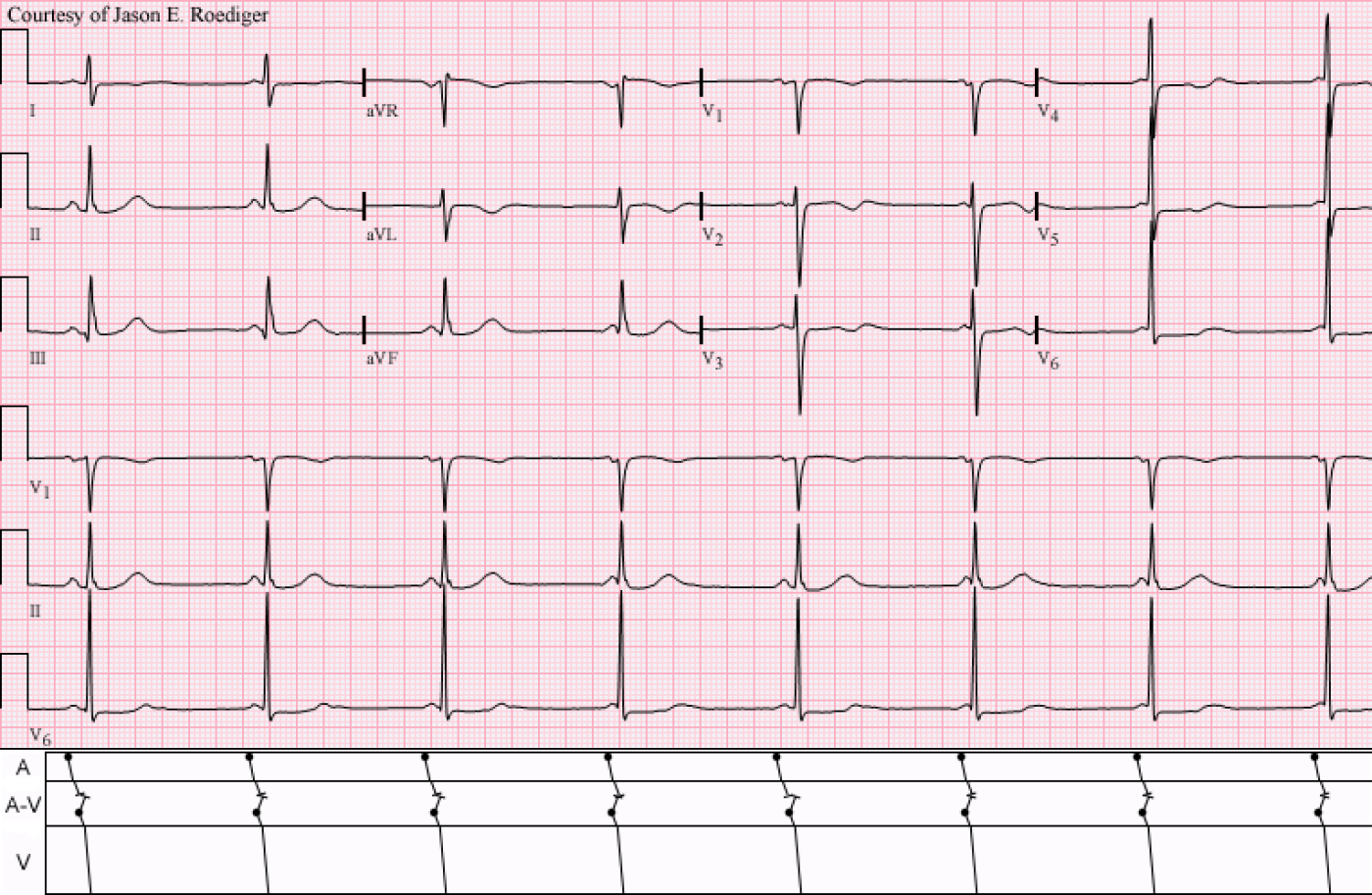
Subsequently, the offending drug (i.e., Atenolol) was stopped and their sinus rate eventually increased to 62/min with a resumption of normal sinus rhythm at a ratio of 1:1. This was seen in the bottom ECG which was recorded 7 days later.
Sources/References:
1. Marriott HJL. Practical Electrocardiography. 8th ed. Baltimore: Williams & Wilkins, 1988, p. 114 & 342.
Jason E. Roediger - Certified Cardiographic Technician (CCT)
[email protected]
Thank You Jason!
Nice explanation to this tracing Jason! You always have a few surprises (I would not have thought this tracing to be confused with WPW ... ). As per your laddergram - I think an additional point to emphasize is that despite AV dissociation - there is NO evidence of any AV block on this tracing (ie, we have no idea whether P waves would conduct if given the chance to do so). THANKS for posting! - : )
Ken Grauer, MD www.kg-ekgpress.com [email protected]