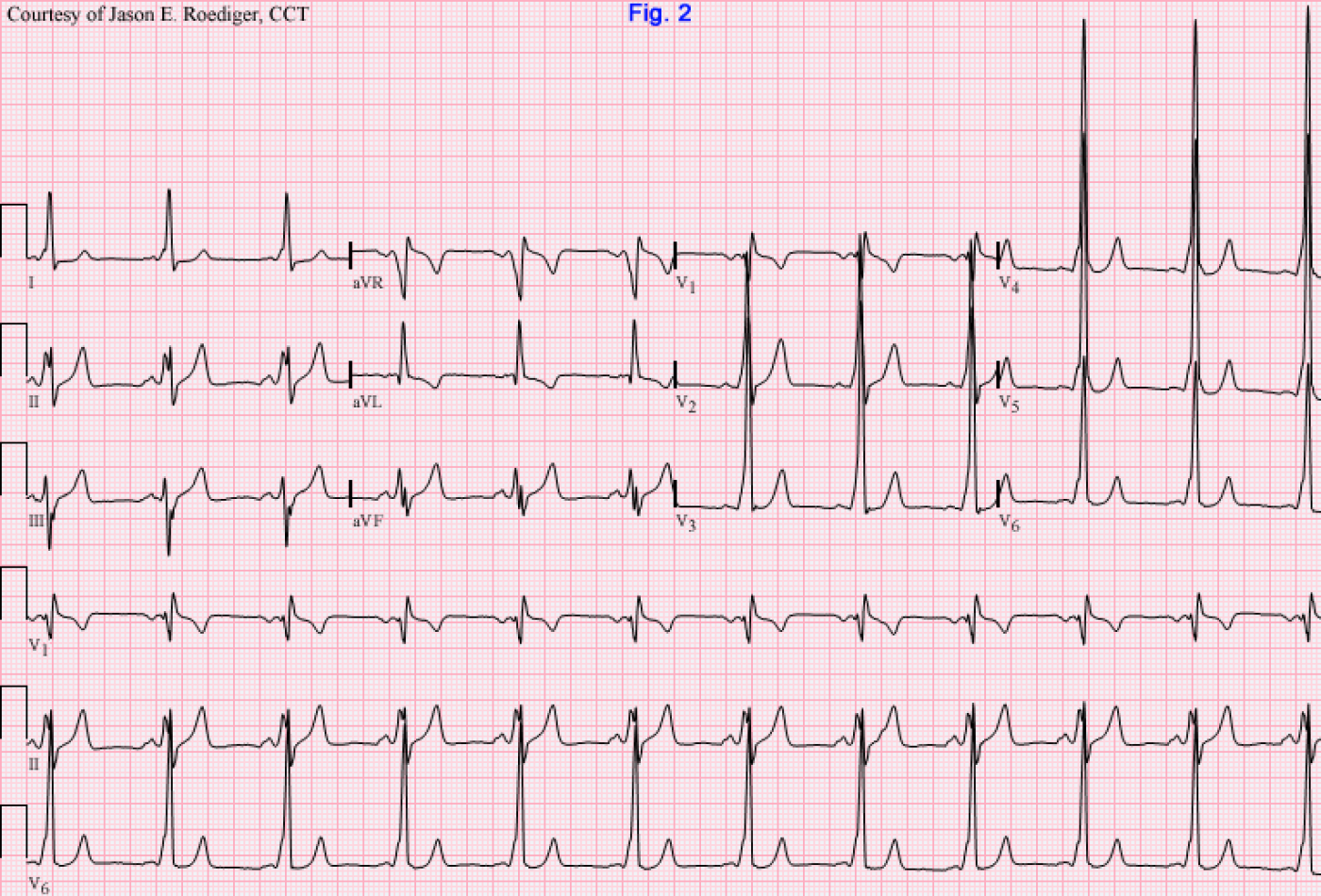
Found this "gem" buried deep-down in the back of the vault and have wanted to share it for many months. Due to the impressive QRS voltage and overlapping waveforms, I initially debated on whether or not I should post this at 1/2-standard but in the end I decided to retain its original size. This ECG is from 27 years ago so I have very limited information, but this is what I do know.
Patient's clinical data: 37-year-old white man who presented to the emergency room in this rhythm. Since he had no prior serial ECGs to compare this to, this ECG was serving as his "baseline".
Questions: What is the source of this mechanism and what might you expect to see once the patient's "normal" rhythm was restored? Would you give verapamil for this rhythm?
-
- jer5150's blog
- Log in or register to post comments
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.



Comments
Left Posterior AP
I think this is preexcited atrial fibrillation. Shortest V to V is less than 200 ms. This puts him at high risk for SCD. If clinically stable, Procainamide IV. If not, then DC CV. Next step is ablation as an in-patient.
This ECG is quite scary! Upon
This ECG is quite scary! Upon a closer look, we can conclude that this is an IRREGULAR WIDE COMPLEX TACHYCARDIA.
Irregular because there is beat to beat variability(RR variability is seen throughout the entire tracing)
Wide because the QRS duration is more than 3 small boxes or 120 ms
Tachycardia because heart rate is more than 100 beats per minute
When there is no discernible atrial electrical activity(P waves) seen, or when you are unsure whether they are present. There are 4 differential diagnosis that you will need to consider when it comes to irregular WCT
1)AFib with wide QRS as a result of aberrant conduction or pre-existing bundle branch block
2) AFib with an accessory pathway(WPW)
3) Polymorphic VT or Torsade De Pointes(if there is documented QT prolongation)
4) Normal VT
The conventional teaching is that when you see a wide complex tachycardia, think about VT,VT and VT first before anything else especially when it is regular
4) Although VT can sometimes be slightly irregular, we exclude this from our differential diagnosis because of the marked persistent irregularity seen in this tracing. If you can appreciate in the long rhythm strip, some of the RR interval is twice the duration of others(some of them is approximately 2 big box some of them is 1 big box)
3) we rule out polymorphic VT or Torsade because the QRS morphology looks quite consistent throughout. And there is no twisting of the axis too!
1 and 2 can be difficult to differentiate. The importance of differentiating lies in the fact that normal AV nodal blocking drugs used recommended for controlling ventricular response of AFib are CONTRAINDICATED because they will accelerate conduction down the accessory pathway precipitating hemodynamic compromise
If this is AFib, the rate is much faster than usual...200 to 300 per minute in various parts of the tracing. The RR interval appears to be in between 1 to 1.5 big box in most part of the tracing. This rate is just too fast for normal conduction to occur down normal AV pathway(the AV node is like a red light in the conduction system and it usually does not allow more than 200 impulses to be conducted each time). Therefor, there must be a bypass tract in the heart that allows impulses to bypass the AV node. Some say if you find AFib with wide QRS at an exceedingly fast rate..consider WPW syndrome
I can't remember the Specific treatment for this as most beta blockers and CCB are contraindicated.Procainamide seems to be quite effective BUT ACLS recommends expert consultation(which I think should be done ASAP) and a synchronized cardioversion should den done at any point the patient becomes unstable.
Changes when normal rhythm is restored. shortened PR,widened QRS complexes, delta waves
WPW with Very Rapid AFib
Excellent points by Dr. RShama & CheeYongChuan (both of whom make Jason's job easy). CheeYongChuan covers highlights in excellent fashion. I'll add just a few points:
GREAT tracing from the "endless" files of Jason Roediger!
Ken Grauer, MD www.kg-ekgpress.com [email protected]
I actually think the first 1
I actually think the first 1/3 of the ECG shows atrial flutter with 2:1 conduction and pre-excitation. It looks to be pretty regular at 150 bpm. From about the 1/3 point it seems to devolve into 1:1 conduction, which continues to devolve either into atrial fibrillation with 1:1 conduction or just atrial flutter with variable conduction down the AVN and AP.
Otherwise I agree with everything else!
Christopher
sixlettervariable.blogspot.com
ems12lead.com
INTERPRETATION
INTERPRETATION (fig. 1):
Atrial fibrillation (rate about 231/min) with A-V conduction via a presumably left-sided accessory pathway (W-P-W syndrome).
INTERPRETATION (fig. 2):
Sinus rhythm (rate = 67/min) with A-V conduction via a presumably left-sided accessory pathwasy (W-P-W syndrome).
COMMENTS:
In fig. 1, the marked irregularity makes ventricular tachycardia unlikely.
The fact that some cycles represent a rate of precisely 300/min (a rate rarely seen in ventricular tachycardia and much more likely to be due to accessory pathway conduction).
Sure enough, 1 hour and 10 minutes after treatment, the ECG in fig. 2 now shows normal sinus rhythm with obvious W-P-W.
To sum up: Always strongly suspect preexcited atrial fibrillation if a wide-complex tachycardia is seen in the presence of profound irregularity; but diagnose it, only if that same preexcited pattern is seen following the restoration of sinus rhythm.
SOURCES/REFERENCES:
(1) Marriott HJL. Challenging ECGs. Philadelphia: Hanley & Belfus, 2002, p. 146-147.
(2) http://europace.oxfordjournals.org/content/7/1/28.full.pdf
Addendum: Christopher Watford does bring up an intriguing point about the possibility of this being atrial flutter. I don't presume to know whether or not that diagnosis was ruled in or out by the electrophysiologist. In the absence of any visibly discrete flutter (F) waves during the longest R-R intervals, I'm going to go with the safe assumption that this is atrial fibrillation. Whichever mechanism of atrial tachyarrhythmia is at work here, verapamil would be contraindicated since it could cause this to deteriorate into ventricular fibrillation
Jason E. Roediger - Certified Cardiographic Technician (CCT)
[email protected]