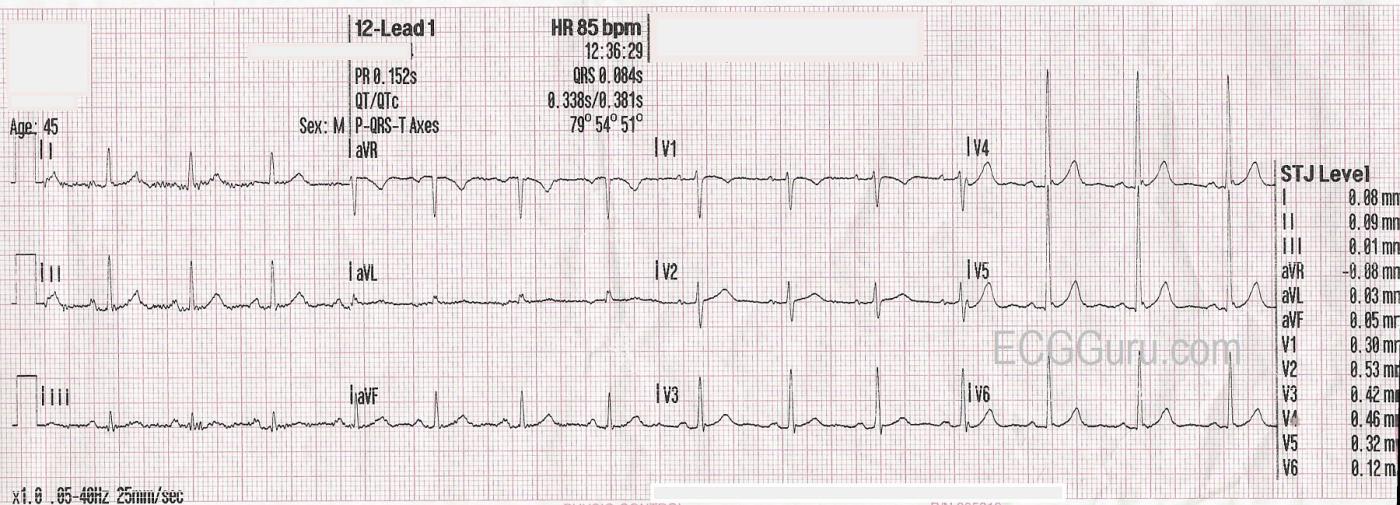
From time to time, we like to publish an ECG that is "within normal limits". While ECGs each look slightly different, there are defined parameters that are considered to be normal. Using the taxonomy terms in the Scrollable List provided on this site, you can easily find and compare the "normal" ECGs. This is taken from a 45-year-old male with a lean body type.
A few of the characteristics that make this ECG normal include, but are not limited to:
* Rate 85 bpm. Rhythm regular. P waves present before QRS complexes. NORMAL SINUS RHYTHM.
* All intervals within normal limits, including a narrow QRS.
* No pathological ST segment elevations, depressions, or Q waves.
* Frontal plane axis is normal. Slightly early R wave transition in the precordial leads.
* No ectopic beats or pauses.
It is very important for students to become familiar with normal ECG characteristics before they learn abnormalities. The normal features become a "template" for the interpreter to compare abnormal ECGs to.
Our thanks to David Morris, Palm Beach County Fire Rescue, for the donation of this ECG.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
What Goes Into a "Normal" Tracing?
I completely agree with Dawn that it becomes RARE these days that we see a "normal" ECG on the internet — because we like to use the internet to highlight the abnormal ECG findings we encounter. And since we see normal tracings much less often on the internet — it may become more difficult to recognize "normal" when we see it. So it is good to periodically talk about "What is normal?" I focus my comments on some ECG features that often pass unmentioned and unnoticed — that I believe are worthy of discussing
Along the way to describing what is "normal" — we need to be systematic, or else findings will be missed. I emphasize that clinical ECG interpretation consists of 2 STEPS: i) Descriptive Analysis (in which we simply describe what is seen — as Dawn has done for today's tracing); and ii) The Clinical Impression (which is based on the descriptive findings we saw in Step #1 — that we now interpret IN THE CONTEXT of the clinical history).
So — We are told that today's ECG is from a "45-year old man of lean body type". However, we are not told the reason that this ECG was obtained. Was it "routine" as part of a physical exam in a healthy and asymptomatic patient? Was it as a baseline in a patient with hypertension? (which IS relevant — as we'll see momentarily). Or was this 45 year old man in the ED for evaluation of new-onset chest pain? (in which case we NEED to know when the chest pain began? How long it lasted? and most important — Was it present AT THE TIME this ECG was obtained, since if chest pain has resolved, then a "normal-looking ECG" could reflect "pseudonormalization" in between the phase of ST elevation evolving into ST depression/T wave inversion that is seen with reperfusion). BOTTOM LINE: Optimal clinical ECG interpretation is impossible without a brief, relevant history — and we have NO HISTORY in today's case.
There is significant baseline artifact in the limb leads. While still able to interpret this tracing — I favor noting the presence of artifact in your descriptive analysis — because if artifact is preventing me from seeing important ischemic findings — I want to document that it is "not MY fault" for missing this. If artifact is obstructing adequate interpretation in a patient with acute symptoms — then REPEAT the ECG (I can't tell you how many times providers fail to repeat the ECG despite artifact that prevents adequate interpretation).
Often ignored are FILTER settings. These are noted in today's tracing (in the lower left corner, below the ECG) — and indicate that a setting = .05-40 Hz was selected. It should be emphasized that this 0.5-to-40 Hz setting is generally used in "monitor mode" — which is the mode typically selected for monitoring of the heart rhythm (because it minimizes artifact and baseline wander that are more likely to affect rhythm interpretation).
In contrast — when assessing for ST-T wave changes — "diagnostic mode" is preferred, for which the recommended filter setting of 0.05-to-150 Hz is recommended to enhance accuracy of ST-T wave analysis. These parameters are probably not clinically important in today's case because of how normal this ECG appears — but as I discuss in My Comment in the 1/13/2024 post in Dr. Smith's ECG Blog (at the bottom of that page —
https://hqmeded-ecg.blogspot.com/2024/01/orthostatic-hypotension-onset-a... ) — there ARE times when selection of certain filter settings can profoundly alter what we are and are not able to see on an electrocardiogram. So it is important to always LOOK for what filter setting was used.
I count 25 mm for height of the R wave in lead V5. In this 45-year old man — this DOES satisfy voltage criteria for LVH. This could be relevant information IF this was a hypertensive patient and the reason this ECG was being obtained was as a baseline, and to assess for likelihood of LVH (ie, Is an Echo indicated?). (For more on "My Take" re assessing LVH on ECG — Please check out my ECG Blog #73 — https://tinyurl.com/KG-Blog-73 ). I'll emphasize that the presence of voltage for LVH in the absence of a reason to have LVH (ie, no hypertension; no heart failure) and in the absence of ST-T wave changes of LV "strain" is not at all specific for true chamber enlargement — but then again, we do not know the reason this ECG was obtained.
Finally — there IS slight ST elevation in leads V4 and V5. That said — the slope of the ST segments in these leads is upsloping ( = "smiley"-configuration) — the QTc is not increased — and there are no abnormal ST-T waves in other leads. It's important to note that there is J-point notching in both of these leads (V4,V5) — which together with the other features just mentioned strongly suggests this is a normal repolarization variant. Awareness to look for this J-point notching, QTc duration, ST-T wave changes in other leads is helpful in cases when less certain if ST elevation is likely to be benign.
In summary — depending on the history in today's case — this ECG is likely to be "normal" with the exception of voltage for LVH (which more likely than not does not correlate with true chamber enlargement).
P.S. I realize my above discussion is long. In "real life" — it takes me seconds to consider all of the above factors along the way to my final interpretation. The reason I can do this so fast — is the result of many years of systematic interpretation with clinical correlation.
Ken Grauer, MD www.kg-ekgpress.com [email protected]