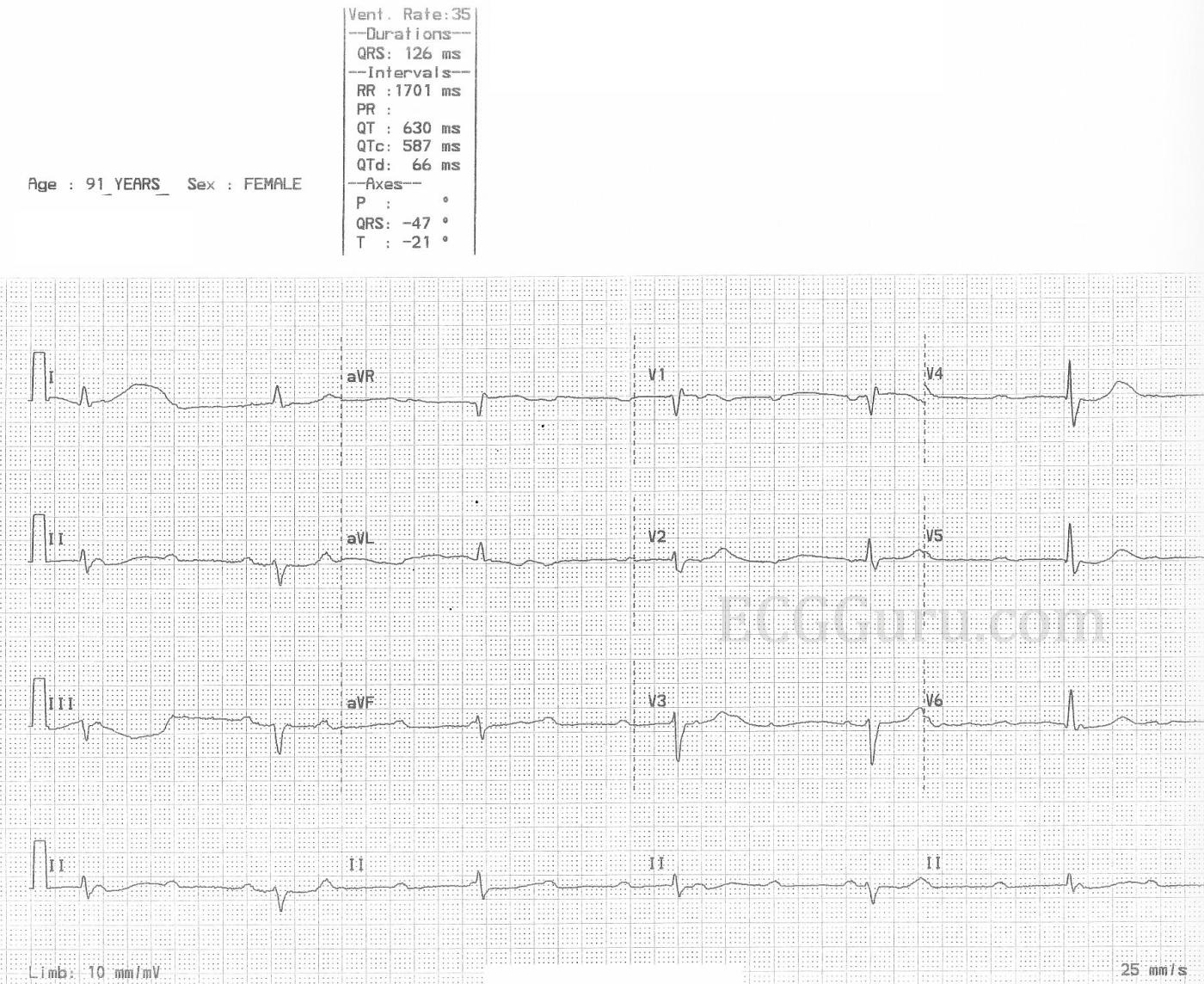
The patient: This ECG was obtained from a 91-year-old woman who was complaining of weakness. Unfortunately, we have no other information.
The ECG: This ECG has something for your basic students, and even more for the more advanced learners. The first thing that anyone should notice is the slow rate. The ventricular rate is around 35 bpm, and regular. If the patient is showing signs of poor perfusion, we would stop here and prepare to increase the rate with a temporary pacemaker (transvenous or transcutaneous). Why is the rate so slow? There is no P wave in front of each QRS, so this is not sinus bradycardia. Rather, we see P waves at a rate of approximately 100 bpm, wit a very regular rhythm. Beginners should “march out” the P waves with calipers or by marking a straight edge piece of paper. There are 15 P waves on this ECG – some are buried within QRS complexes (QRS #3) or T waves (QRS #4).
Because there are two distinct, regular rhythms, but they do not track with one another, we know this is possibly third-degree AV block (complete heart block). Another clue is that there are no steady, repetitive PR intervals, which means there is no relationship between the atrial rhythm and the ventricular rhythm.
For more advanced learners, it is helpful to try to identify the origin of the escape rhythm. If it is junctional, the AV block is above the junction. If the escape is ventricular, the AV block is below the junction. A junctional rhythm is usually between 40 – 60 bpm, with a narrow QRS. Ventricular escape rhythms are usually less than 40 bpm and with wide QRS complexes. This ECG will be a little challenging on this front, because the rhythm has some characteristics of junctional rhythm and of ventricular rhythm.
· The QRS is wide. Normally, that finding favors the diagnosis of ventricular rhythm, but interventricular conduction delays like bundle branch block can widen a junctional QRS. There is a small R’ in V1 and a wide little S wave in I and V6, favoring the diagnosis of right bundle branch block.· The frontal plane axis is abnormal. This can be a sign of a ventricular rhythm, because the axis reflects the direction of the electrical flow in the ventricles. But, this left axis deviation is also seen in left anterior fascicular block, which is frequently paired with RBBB.· The slow rate is just about on the border between the intrinsic rates of the junctional and ventricular pacemakers. For those who care for patients in an emergency or primary care setting, it is important to emphasize that the origin of the block is not as important as supporting the patient’s need for rate as part of the important cardiac output equation. Another consideration for this patient is “what caused the AV block”? She is very old, and that certainly is a factor. But, on close inspection, we see ST changes. Specifically, there are flattened, slightly depressed ST segments in II, III, and aVF. AVR has the same flat shape, with some elevation. V1 has a very subtle ST changes, as well. This is a sign of diffuse ischemia (chronic or acute). The machine read the QTc as prolonged, but I measured using an online measuring tool, and got 464.8 with the Bazett equation.
ECGs should always be approached in a systematic manner. When possible, patient presentation and symptoms should inform one’s decisions.
EDIT: Please read the comment below from David Richley and Ken Grauer. They bring up a very good argument for "high-grade" AVB, which is a good conversation to have with more advanced students.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Complete or almost complete?
Yes, there is heart block here but is it DEFINITELY complete? Maybe, but I just wonder if it might possibly be high-grade AV block with occasional conducted beats. Two of the beats – 2 and 5 – have QRS complexes that are different in shape from the rest. They are predominantly negative in lead II, where the rest are equiphasic or slightly positive, and they have a QRS that is predominantly positive in V2 whereas the others have slight overall negativity.
These two beats are also distinguished by ending relatively short RR intervals – 1600 ms in each case rather than 1640 or 1680 ms. So, could beats 2 and 5 be conducted beats, and the rest junctional escapes? If so, why would these 2 beats conduct when the rest cannot? It could be down to the RP interval. Perhaps, if the RP interval is long enough, the AV node has had sufficient time to recover and permit conduction. The RP intervals of the 2 beats with a different morphology are 1340 and 1400 ms, and these intervals are much longer than any of the others on the ECG. However, if these 2 beats are conducted, wouldn’t they be expected to have the same PR interval? Here the PR intervals are 260 and 200 ms but this difference can be explained again by the RP interval – the longer the RP interval, the better the AV node is able to conduct and therefore the shorter is the PR interval of conducted beats. This phenomenon is known as RP/PR reciprocity. Here an RP of 1340 ms is followed by a PR of 260 ms and an RP of 1400 ms is followed by a PR of 200 ms.
Maybe I’ve got an overactive imagination and this really is just complete heart block,
with the slight irregularity in ventricular rate perhaps due to autonomically mediated variation in the junctional discharge rate, analogous to what is seen in sinus arrhythmia, although I’m not sure this explains the different QRS morphologies.
Thanks so much, Dave, for
Dawn Altman, Admin
High-Grade But NOT Complete AV Block
This is a fascinating arrhythmia case with teaching points for every level provider. For less experienced clinicians — I’d be happy if their interpretation was “bradycardia with a rate in the 40s, and either high-grade or complete AV block in a symptomatic 91-year old who will probably need a pacemaker.” After all — what is important, is to recognize the severity of this bradyarrhythmia, with awareness of optimal management concerns (ie, admission to the hospital to rule out recent or acute infarction, hypothyroidism, electrolyte disturbance and/or overuse of rate-slowing antiarrhythmic medications).
I’d add “extra credit” for providers recognizing the low voltage — incomplete RBBB with LAHB — and clearly abnormal ST-T waves showing diffuse ST segment flattening with slight depression, in association with ST elevation in lead aVR > V1. More advanced providers should recognize this pattern of ST flattening and depression in multiple (more than 6) leads with ST elevation in lead aVR (and sometimes in V1) — as indicative of diffuse subendocardial ischemia. Advanced providers should know that in addition to severe coronary disease — that other entities might also produce an ECG pattern consistent with diffuse subendocardial ischemia (ie, anemia, electrolyte disturbance, hypoxemia, “sick patient”, etc.) — but given the age of this patient and the severe conduction disturbance, the likelihood of severe underlying coronary disease (albeit not necessarily recent infarction) is high.
And then there is the fascinating cardiac rhythm! On this — I completely agree with David Richley that this rhythm almost certainly is NOT complete AV block. I say this with full awareness that it is impossible for Dave and myself to prove from this single rhythm strip, that today’s rhythm is some complicated form of 2nd-degree, but NOT complete AV block.
Why then am I so sure? My attached laddergram shows my proposed theory. I’ve taken Dave’s measurements, and developed what I believe can be a plausible mechanism. I have NO doubt that variations on my laddergram are possible — but the “theme” of my proposed mechanism suggests 2nd-degree AV block with significant bradycardia because we see an underlying regular atrial rate (RED arrows) with multiple P waves that should conduct, but fail to do so.
The reasons I am all but certain that this rhythm is not complete AV block are: i) That the R-R interval (as per Dave’s measurements) is not equal (as it most often is with complete AV block); — and — ii) That there are 2 different SHAPES of QRS complexes (as per Dave) — with the preceding R-R interval before one of these shapes (ie, before beats #2 and 5) being precisely equal ( = 1,600 msec.). This is highly unlikely to be due to chance! On the contrary — one of the BEST clues I have found over the years for distinguishing between conducted vs junctional escape beats — is that QRS morphology may differ slightly for junctional escape beats compared to QRS morphology for sinus beats (felt to be the result of the impulse not necessarily arising from the same point within the AV node for junctional escape beats, compared to the path of normal sinus-conducted beats.
I illustrate my proposed mechanism with a laddergram. Regarding laddergrams — these can take some time to learn to draw — but they are EASY to understand (My ECG Blog #188 (https://tinyurl.com/KG-Blog-188 provides numerous detailed illustrations for those interested in understanding and/or learning to draw laddergrams).
That said — I found today’s arrhythmia especially challenging to draw because: i) There are no repetitive R-R intervals; ii) There appears to be dual-level AV block ( = a complex concept that I explain and illustrate in detail in my ECG Blog #347 = https://tinyurl.com/KG-Blog-347 ); and iii) While not all the same, R-R intervals are of comparable length, such that there are no “easy” answers regarding which beats are conducted by which P waves.
As a result of this challenge — I had to guess which beats might be conducting — and then try to work this out in a plausible fashion (ie, drawing this laddergram took me much longer than it usually does). I knew beats #2 and 5 were junctional escape beat (for the reasons I cite above) — and I knew that with dual level AV block, there is usually some form of Wenckebach conduction — but because of the ever-changing PR intervals, there was no “predictable” pattern.
BOTTOM LINE: As I stated earlier — there is something to learn from today’s case for every level provider. I’m happy if a complex and severe form of 2nd- or 3rd-degree AV block is recognized — with realization of the probable need for a pacemaker. And for those who love solving complex arrhythmias — this is a “fun” tracing to try your hand at. I welcome those who come up with alternative solutions to the one I propose in my laddergram.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Conducted vs escape beats
It’s interesting that Ken and I agree that this is probably high-grade rather than complete AV block, and for the same reasons, yet the beats that I think are conducted, Ken thinks are escape beats and the beats that I think are escape beats, Ken thinks are conducted. Ken’s laddergram and explanation show very nicely that complex arrhythmias often have multiple plausible explanations and it may be difficult if not impossible, on the basis of a single ECG, to determine which is the correct one.
Whenever I see what looks like high-grade AV block with an irregular ventricular rate I always assume that the relatively early beats are conducted and the those that end longer RR intervals are escapes because this seems to make the most sense. In Ken’s explanation the 2 escape beats emerge after an interval of 1600 ms, but if this is the escape interval, why are there longer RR intervals that are not terminated by escape beats? For instance, looking at the laddergram, it seems to me that if Ken is correct that beat 2 is an escape beat, then there should be another one after a further 1600 ms rather than the conducted beat that occurs after an interval of 1680 ms.
So, I’m sticking with my explanation for now, but it’s entirely possible that there is a better, more plausible explanation still waiting to be revealed.
Laddergram Debate — and What Really Matters ...
To no surprise — I believe David Richley and I agree about “the forest” — but we have different opinions regarding a few of "the leaves" that are on “the trees”. This is FINE — since our years of interpreting the most challenging of arrhythmias have provided us both with the perspective of fully recognizing (and welcoming) the reality that there may be more than one plausible explanation to any given arrhythmia.
In today’s case — the KEY (missing) finding, is understanding WHAT the “normal” ( = sinus-conducted) QRS complex in a long lead II rhythm strip should look like — because then we would KNOW which of the 2 slightly different shapes in today’s tracing (ie, beats #2,5; vs beats #1, 3,4; 6) is sinus-conducted — and which represents junctional escape.
I suspect that either a glance at a prior tracing when the patient was in sinus rhythm OR an additional 20-30 seconds of monitoring immediately after the recorded ECG we are analyzing today — may have supplied us with a definitive answer.
I agree completely with Dave that one of the BEST clues to tell us that a given beat in a high-grade block IS being conducted — is when the beat occurs earlier-than-expected (and this concept weighs against my theory that beats #2 and 5 with shorter preceding R-R intervals are not conducted). That said — I thought my laddergram does explain this shortcoming (ie, the longer PR interval of the 5th beat — and concealed conduction from other blocked impulses temporarily suppresses the AV nodal pacemaker) — but I realize this is a bit of a ”stretch”.
That said — another KEY concept in working out complex high-grade block mechanisms, is that the R-R intervals of escape beats are usually quite constant (since escape pacemakers are usually, albeit not always — quite regular). But Dave’s theory invokes calling beats #3,4 and 6 escape beats — and the preceding R-R intervals for these beats is not the same (ie, 1680 vs 1640 msec.).
BOTTOM LINE: There are “holes” in both of our theories — that I believe we both acknowledge. Given the peculiarities of today’s tracing (ie, lack of any repetitive PR intervals; 2 sets of identical R-R intervals, but also an “orphan” [1640 msec.] interval; and no “tell-tale” clearly earlier-than-expected QRS) — I submit that there is NO way to know for certain what the precise laddergram for today’s rhythm is.
That said — I will reword the “Take-Home” message that I hoped to convey from my initial Comment. There IS something for providers of ALL levels to learn from today’s fascinating arrhythmia. An important message that is all-too-often overlooked (which Dave and I both know only too well) — is that sometimes we just do not have enough information from a single rhythm strip to know for sure what the precise explanation is. It is important to appreciate and ACCEPT THIS CLINICAL REALITY. Practically speaking — NONE of this matters, because in this symptomatic 91yo who manifests diffuse subendocardial ischemia on her 12-lead — WHAT COUNTS is simply that she has symptomatic bradycardia with some complex form of 2nd-degree (or possibly 3rd-degree) AV block — and that after an acute event and “something fixable” are both ruled out — that this patient most probably will benefit from a pacemaker.
Hopefully interested readers will benefit from this “Take-Home” message — fully appreciating that nearly a century of arrhythmia interpretation experience between Dave and myself is still not enough for us to agree on a single laddergram. But this is OK — because we both appreciate what optimal management for this patient will be.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
I don't know what else to add to this conundrum!
I thought that Drs. Richley and Grauer had pretty much exhausted the possibilities here, but while looking at Ken's laddergram, another thought came to me.
The two beats that Ken felt were PJCs may be more than that. What if Ken had only laddergrammed the PJCs that were manifest - but others were concealed? I did not create a separate laddergram, but just added a bit to Ken's. What do the three of you think of the possibility that there is a junctional parasystole and we are seeing only those beats that manage to conduct to the ventricles? It may take a bit of minor readjustment of the laddergram, but I think that is a possibility which could also explain the different QRS morphologies as well as the different R-R intervals.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
Incorrect Example...
Sorry - my additions did not transfer to the JPG. Let's try once more.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
OK... this is it! Third time's charm!
Trying one last time!
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
Theoretically possible but is it likely?
Another layer of complexity! I think Dr Jones’s suggestion is a theoretical possibility but its plausibility just can’t be assessed over such a short time period – we would need a MUCH longer rhythm strip. If beats 2 and 5 are indeed of junctional origin, as Ken also believes, then a parasystolic mechanism, with exit block, might explain the apparently contradictory non-appearance of junctional beats when they might otherwise be expected. And entrance block, protecting the parasytolic focus, might explain why beats 2 and 5 are early in relation to other beats. However, on the basis that high-grade AV block and a junctional parasystole feels like a statistically unlikely combination, I’m sticking with my simpler explanation!
Yes... I think it's likely!
Dr. Richley...
Thank you for your thoughts. I don't think I could have argued in favor of my suggestion any better than your comment.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd