The Patient: This series of ECGs is from a 65-year-old woman who was complaining of a sudden onset of chest pain, nausea, and weakness. She stated that the pain increased on inspiration. She reported a history of non-insulin-dependent diabetes mellitus (NIDDM).
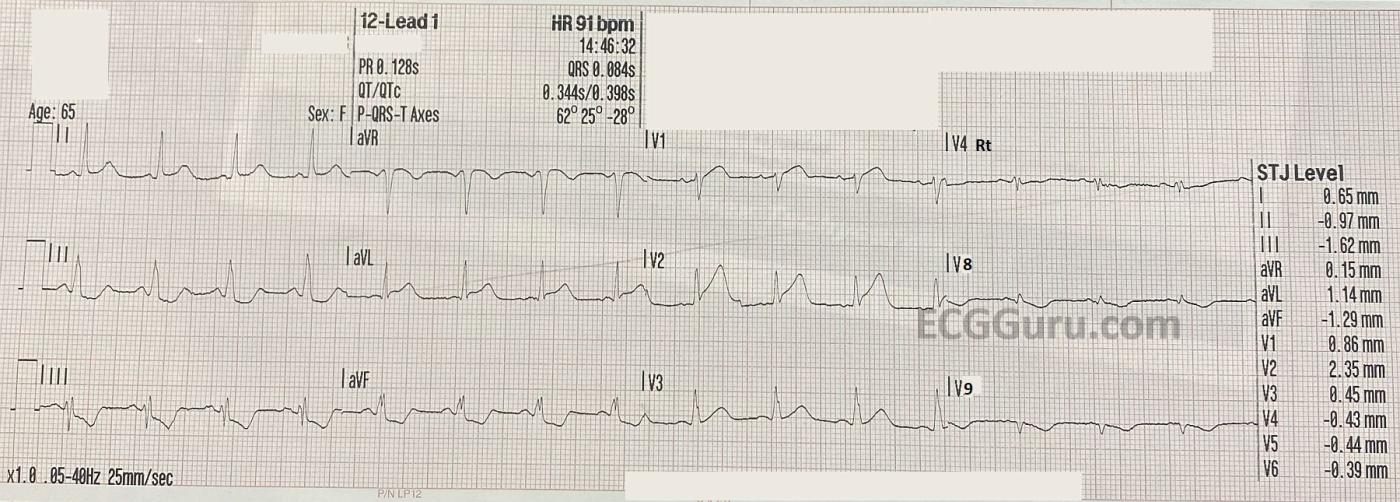
ECG No. 1, 14:46: This ECG includes V4Right, V8 and V9 in place of V4, V5, and V6. The rhythm is sinus at 91 beats per minute. The PR interval is within normal limits, as is the QRS duration. The QTc is WNL as well. The frontal plane axis is also WNL. The three standard chest leads show an early transition of R waves in V2. There are noticeable ST and T wave abnormalities:
slight ST elevation in I and aVL with ST depression in II, III, and aVF. In chest pain, possible M.I., STD should be presumed to be reciprocal in nature. V1 has slight STE with a coved upward (frowning) appearance. V2 has more noticeable STE, with a tall, wide-based T wave. This is called a “hyperacute T wave”. We will have to evaluate V4 – V6 on ECG No. 2.
V4 Right has no ST elevation, and V8 and V9 have ST depression (reciprocal to the anterior leads). So far, we have all the signs of acute anterior wall M.I.
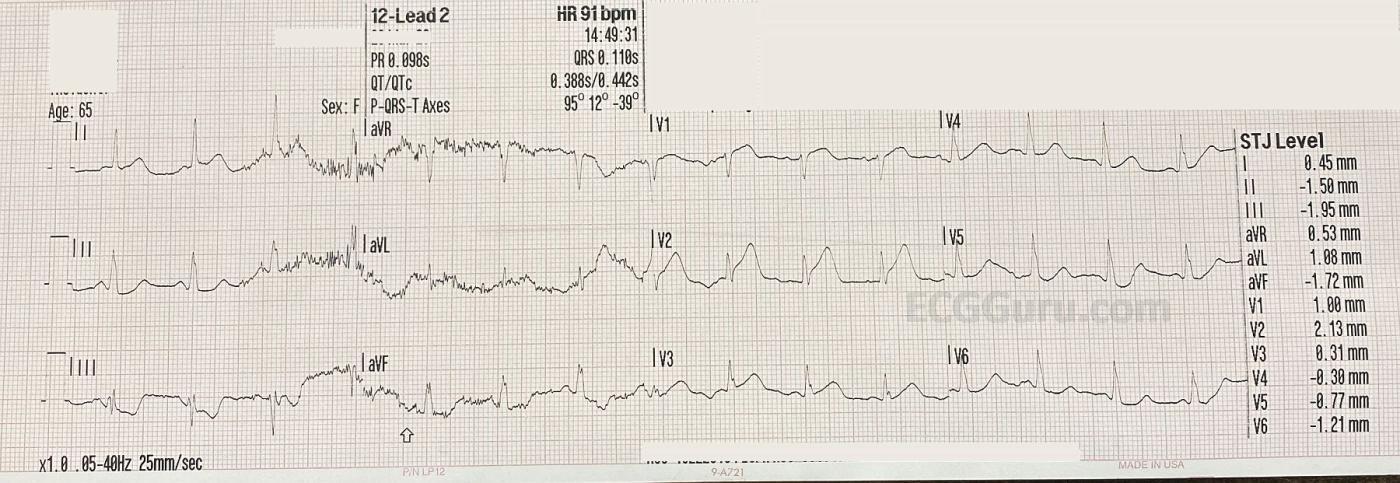
ECG No. 2, 14:49: This ECG, taken three minutes later, includes the 12 “standard” leads. The ST depression in the inferior wall has increased slightly. There is not much change in the anterior STE. There is movement artifact in the first half of the ECG. Leads V5 and V6 show STD.
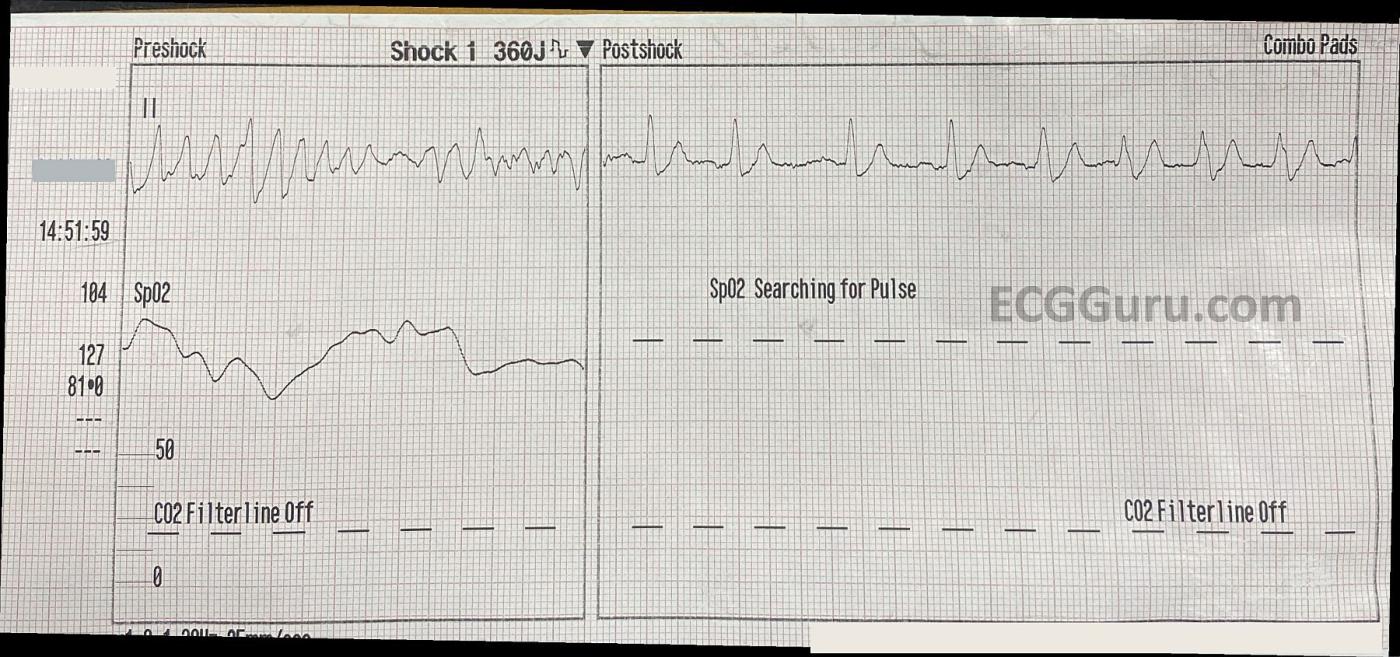
Rhythm Strip at 14:51: Shows v fib, and a 360 J defibrillation that resulted in sinus tach with wide QRS complexes. The rhythm just before the v fib was more “organized” looking, with regular, fast QRS complexes of varying heights, as seen in the first half of the rhythm strip, but this rhythm deteriorated very quickly.
Learning Points: This patient was dramatically symptomatic, but her ECG signs of M.I. might have seemed subtle to the inexperienced viewer. It is important to be very systematic in looking at ECGs, and ST changes particularly. The ECG machine aided us by measuring ST elevations and depressions, and it is easily seen that these signs occur in “related leads”. Localization of ST elevation is a very accurate sign of ACUTE ST ELEVATION M.I. Additional leads should probably be done after the standard 12. RVMI is rare in anterior wall M.I., as the RV is supplied by the right coronary artery, and the anterior LV wall is usually supplied by the left anterior descending artery. Posterior leads can confirm posterior wall M.I. if it is suspected by the presence of ST depression in V1 – V3.
There was some discussion about whether the sudden-onset wide-complex tachycardia could be Torsades de pointes. TdP can only be diagnosed in the setting of long QTc, which was not noted in the first two ECGs. Polymorphic VT in the setting of acute M.I. is usually associated with ischemia, not QT prolongation. It can be very hard to determine the point at which polymorphic VT becomes V Fib, but clinically, it does not matter. The patient needs to be defibrillated.
Follow up: The patient was taken to the cath lab within 45 minutes of EMS patient contact. She was found to have a proximal 100% occlusion of the left anterior descending branch. Angioplasty was successful, and we have no further information.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.



Comments
Acute Proximal LAD Occlusion — A Case to Learn From
Today's case provides a lot we can learn from. The GOOD NEWS — is that this patient was cathed within 45 minutes of EMS contact — and that PCI successfully reperfused the acutely occluded vessel.
As I always taught throughout my 30-year academic career (and strived to do myself in cases I directly managed) — even when outcome is good, there is ALWAYS much to learn from carefully rethinking cases to see how management might be even better the next time around. So it is with today's case.
For clarity — I have put the 3 ECGs together sequentially in my Figure, in which I label them as ECG #1, #2, #3.
The 1st ECG in today's case was not a complete 12-lead. Instead, critical leads V4,V5,V6 were omitted so that a V4R, V8 and V9 lead could be obtained. This unfortunately was a waste of time — which WAS clinically relevant given that the patient went into VFib just 5 minutes after ECG #1 was obtained. As it turned out — significant artifact impeded interpretation of ECG #2 — such that we NEVER had a complete standard 12-lead ECG on this patient.
WHY do I say it was a "waste of time" to start with a 9-lead ECG + V4R, V8,V9? Simply because there is absolutely NO potential for those leads to provide ANY useful information at all in today's. Leads V8,V9 are aimed at assessing for posterior infarction — but the ST elevation in anterior leads V1,V2,V3 of ECG #1 immediately ruled that out. RV infarction is seen with acute proximal RCA occlusion, that is characterized by associated acute inferior infarction — which clearly was not present in ECG #1 (ie, there is NO inferior lead ST elevation on this tracing).
Had standard leads V4,V5,V6 been done on the initial ECG — then: i) The diagnosis of acute LAD OMI ( = Occlusion-based Myocardial Infarction) could have been definitively reached sooner — potentially expediting cardiac catheterization; and ii) It would have been that more obvious that leads V4R, V8,V9 were most definitely NOT needed (again — this being relevant to today's case given development of VFib just a few minutes later).
The diagnosis of acute proximal LAD occlusion in today's case is NOT subtle. In lead V1 — the ST segment straightening with elevation and ST coving is never normal. In lead V2 — there is significant ST elevation as well as an obviously hyperacute T wave (much taller-than-expected and wider-at-its-base than should be considering QRS amplitude in this lead). More than this — there is T-QRS-D ( = Terminal QRS Distortion — as shown by the BLUE arrow) — which is diagnostic of acute coronary occusion (Please see my ECG Blog #318 for discussion of this important ECG sign = https://tinyurl.com/KG-Blog-318 ). Lead V3 continues with a hyperacute T wave. Lead aVL in ECG #1 shows ST elevation — with marked reciprocal ST depression in each of the inferior leads. In this patient with severe new chest pain — this is absolutely diagnostic of acute proximal LAD occlusion! Immediate cath for prompt reperfusion is essential for optimal outcome.
ECG #3 — shows 3 seconds of what I would interpret as coarse VFib. As per Dawn — the diagnosis of Torsades de Pointes is dependent on QTc prolongation, which is not present in today's case. To me — we don't see persistence of this rhythm long enough to call it PMVT (PolyMorphic VT). IV Magnesium is not a treatment of choice for what I see on today's tracings. Instead — this is ischemic VFib from an extensive proximal LAD occlusion in need of immediate defibrillation — followed by PCI as soon as this can possibly be done.
The outcome in today's case was good! It's easiest to take this hard critical retrospective look at each step in today's case when there is a LOT that was done well! This was the case here — as it is NOT easy to get the patient to the cath lab within 45 minutes of EMS contact! That said — the lessons to be learned here will hopefully help to make management that much better in future cases.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Link To Dr. Grauer's discussion on TERMINAL QRS DISTORTION
Dawn Altman, Admin