The Patient: A 64-year-old man complaining of chest pain and shortness of breath for 20 minutes. Long-standing history of triple vessel disease, severe aortic stenosis, hypertension, thrombocytopenia. Meds unknown. He was not considered to be a candidate for valve surgery.
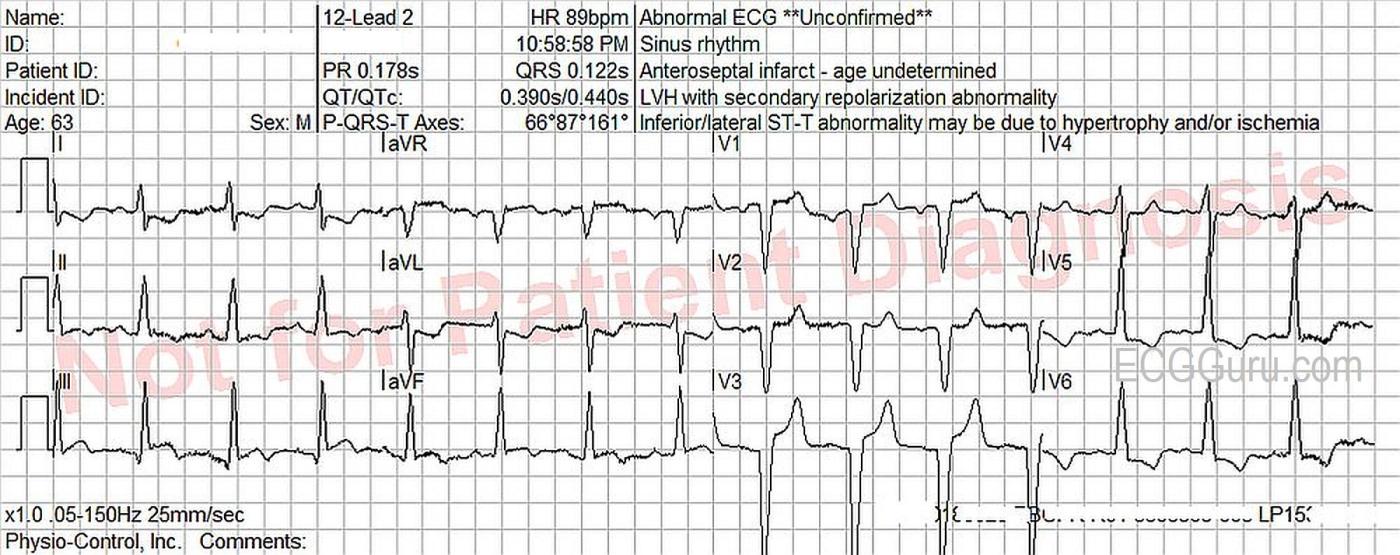
The ECG: There is normal sinus rhythm with a rate of 90 bpm. P waves are not visualized well in all leads, so remember that the three channels of this ECG are run simultaneously. If you see a P wave in Leads I and II, they are also present in Lead III. The PR interval is WNL.
The QRS complexes are wide, at .122 seconds (122 ms). The criteria for left bundle branch block are met. (Supraventricular rhythm, wide QRS, upright QRS in Leads I and V6, negative QRS in V1). The frontal plane axis is within normal limits, but toward the right, at 87 degrees. The QRS complexes transition at V4 from negative to positive, but Leads V1 – V3 have no initial r waves. These are possibly pathological Q waves, likely from a past anterior-septal M.I.
In left bundle branch block, and most other conditions that cause wide QRS, there will normally be ST changes. The ST segments will deviate from the baseline in a direction opposite, or discordant, from the QRS. So, all leads with a wide, upright QRS should have some ST depression. All leads with a wide, downward-deflected QRS should have some ST elevation. Further, this ST change is proportionate to the size of the QRS complex. A TALL or DEEP QRS will be accompanied by more ST depression or elevation, while a small or biphasic QRS may show no ST deviation at all.
Because there is normally ST segment deviation with left bundle branch block, it can be tricky to recognize acute coronary syndromes, like M.I. or STEMI. In 1996, Dr. Elena Sgarbossa first described criteria to help clinicians determine the presence of ACS in the presence of wide QRS.
She did not have the advantage of cath lab results to confirm her findings, but the criteria were very useful. In 2012, Dr. Stephen Smith, et al, published a modified version of the Sgarbossa Criteria. Their research included definitive cath lab findings.
This ECG shows definite signs of acute myocardial transmural injury (STEMI). The inferior leads, II, III, and aVF, have ST elevation which is CONCORDANT with the direction of the QRS. Remember, in LBBB, the ST should be discordant, or opposite, the direction of the QRS. Leads I and aVL show concordant ST depression, a reciprocal change seen in inferior wall M.I.
Patient Outcome: As noted above, this patient had an extensive medical history. On admission, he was determined to be in multi-organ failure. He was scheduled for a cath to determine the extent of his cardiac disease and to help develop a treatment plan. In the pre-procedure area, the patient deteriorated, developed acute respiratory failure, was intubated, and succumbed to his disease without having the procedure.
Our thanks to Sebastian Garay for donating this case.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
LBBB/IVCD and Acute OMI in a Patient with CP
Today's ECG is interesting from a number of perspectives. The patient is a 64-year old man who presented with dyspnea and new chest pain. As per Dawn — the rhythm is sinus — and the QRS complex is wide.
There are several potential ways to describe QRS morphology in today's tracing. QRS morphology in the chest leads is clearly consistent with LBBB (ie, all negative in anterior leads V1,V2,V3 — and all positive in leads V5,V6). However, the limb leads are not consistent with LBBB, given a definite S wave in lead I, and a predominantly negative QRS in lead aVL. Although cardiologists may differ regarding the "optimal terminology" — I would favor IVCD (InterVentricular Conduction Defect) for this tracing, given the distinctly atypical appearance of the QRS in the limb leads.
The above said — this type of IVCD "functions like" a LBBB, at least in the chest leads. As a result — it's important to emphasize that NO conclusion can be drawn from the QS complexes in leads V1,V2,V3 regarding the possibility of anteroseptal infarction having occurred at some prior point in time. That's because the initial left-to-right vector of septal depolarization is abolished (by definition) when there is LBBB conduction — and that's the period of time during which Q waves are inscribed on the ECG. We EXPECT to see predominantly negative (if not all negative) QRS complexes in anterior leads with LBBB conduction!
On the other hand — note how the S wave in lead V3 is cut off from the ECG paper! This is clearly a very deep S wave (impossible to tell how deep, given how V3 is cut off). This strongly suggests that in addition to the conduction effect — that this patient has LVH.
How then can we assess for acute ischemia and/or infarction in a patient with LBBB conduction? Dawn alluded to some of the ways, with regard to employing Sgarbossa and/or Modified Smith-Sgarbossa Criteria. None of those criteria are satisfied in today's tracing. Although there clearly is ST elevation in lead V3 — the relative amount of J-point ST elevation in lead V3 is minimal given how deep the S wave is in this lead.
I have always favored "qualitative" rather than quantitative criteria as the most helpful clue for judging acute ischemia or infarction with LBBB or IVCD. These "qualitative" criteria will not always be satisfied — but they ARE in today's ECG. In essence — I look for ST-T wave changes that "should not be there" with simple BBB. The coved and slightly elevated ST segments that end in terminal T wave inversion in each of the 3 inferior leads should simply "not be there" with simple LBBB/IVCD. In support that these are truly acute "primary" ST-T wave changes — is the shape of the ST-T wave "reciprocal changes" that we see in leads I and aVL. To EMPHASIZE — These are subtle changes. But with experience, a comfort level can be reached that in a patient with new chest pain (such as today's patient) — this "shape" of ST-T waves in 5 of the 6 limb leads is immediately recognized as diagnostic of acute OMI ( = Occlusion-based MI) — UNTIL you prove otherwise.
Contrast this with the ST-T wave depression that we see in the lateral chest leads! The ST-T wave depression that we see in leads V5,V6 "looks like" either LV "strain" (from LVH) and/or the typical secondary ST-T wave changes expected with LBBB. The appearance of the ST-T waves in leads V5,V6 is not at all suggestive of ischemia or infarction in this patient with a conduction defect.
For more on "My Take" regarding the ECG diagnosis of BBB, including assessment for ischemia/infarction (using Sgarbossa and other criteria) — Please check out my ECG Blog #282 (https://tinyurl.com/KG-Blog-282) — and ECG Blog #146 (https://tinyurl.com/KG-Blog-146).
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Sgarbossa's criteria
In Ken’s detailed and very helpful analysis of the ECG he says that none of the Sgarbossa criteria for acute MI are satisfied, but is this definitely the case? Although the quality of the recording is not perfect, I am pretty sure that there is at least 1mm of concordant ST elevation in leads III and aVF, as Dawn observes, which would satisfy Sgarbossa’s 1st criterion and make it 88% probable, according to Sgarbossa’s study, that there is an acute MI. Please note that Ken and I don’t disagree at all in our overall interpretation of the ECG, just in the applicability of Sgarbossa’s criteria.