The patient: 79-year-old man complaining of severe “burning” chest pain, radiating to his neck. Walking exacerbates his discomfort. He has had nausea and vomiting for 24 hours. Past medical Hx includes high cholesterol and atrial fibrillation. Medications not known.
The ECGs: These ECGs could be called “classic”. There is a 100% occlusion of the right coronary artery (RCA), which was successfully repaired in the cath lab. About 80% of inferior wall M.I.s are due to occlusion of the right coronary artery. Depending on how proximal the occlusion is, we can expect a pattern on the ECG representing injury to all areas supplied by the RCA. This “package deal” can include:
· Inferior wall ST elevation.
· Posterior wall extension.
· Right ventricular M.I.
· Right atrial ischemia, including damage to the SA and AV nodes.
· Occasionally, low lateral wall ST elevation, when that area is solely perfused by the RCA.
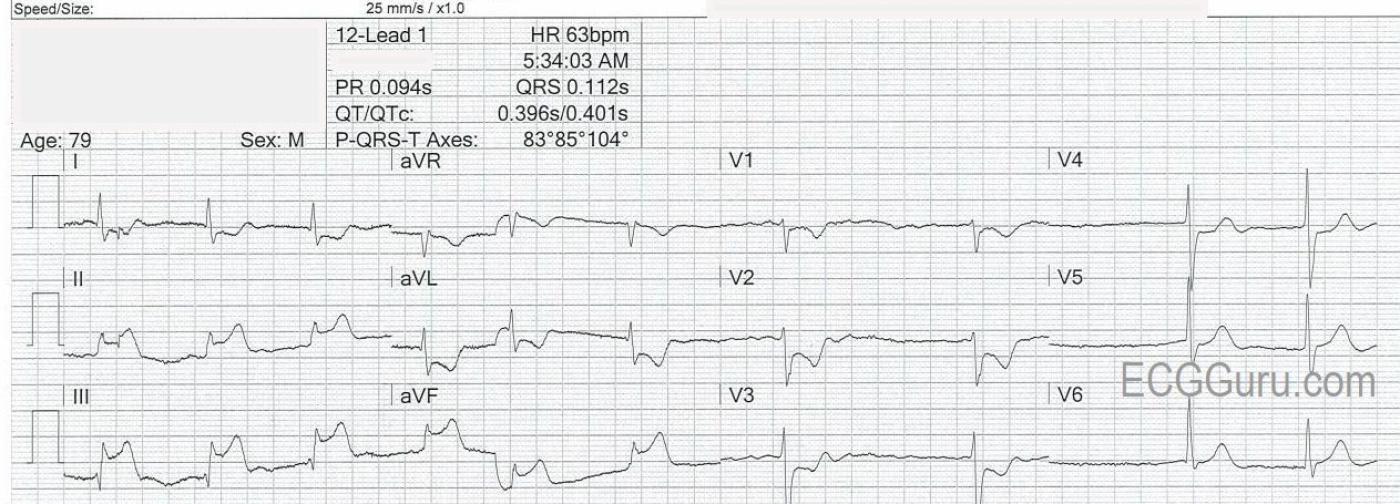
ECG No. 1,obtained at 5:34 am, shows the following:
· Atrial fibrillation with a slow ventricular response. (AV node may be ischemic).
· ST elevation in Leads II, III, aVF, V4, V5, and V6. (Transmural injury in the inferior and low lateral wall).
· Reciprocal ST depression in I and aVL. (Leads reciprocal to inferior wall).
· Reciprocal ST depression in V1, V2, and V3. (Leads reciprocal to posterior wall).
· Hyperacute T waves in leads with STE (often a sign that precedes the STE).
· STE in Lead III is greater than STE in Lead II. STD in V1 minimal, compared to V2. (These are reliable signs that there is right ventricular M.I.)
From this list of ECG signs, we can say that there is INFERIOR WALL ST ELEVATION M.I., plus likely RIGHT VENTRICULAR M.I. and POSTERIOR WALL EXTENSION OF IWMI.
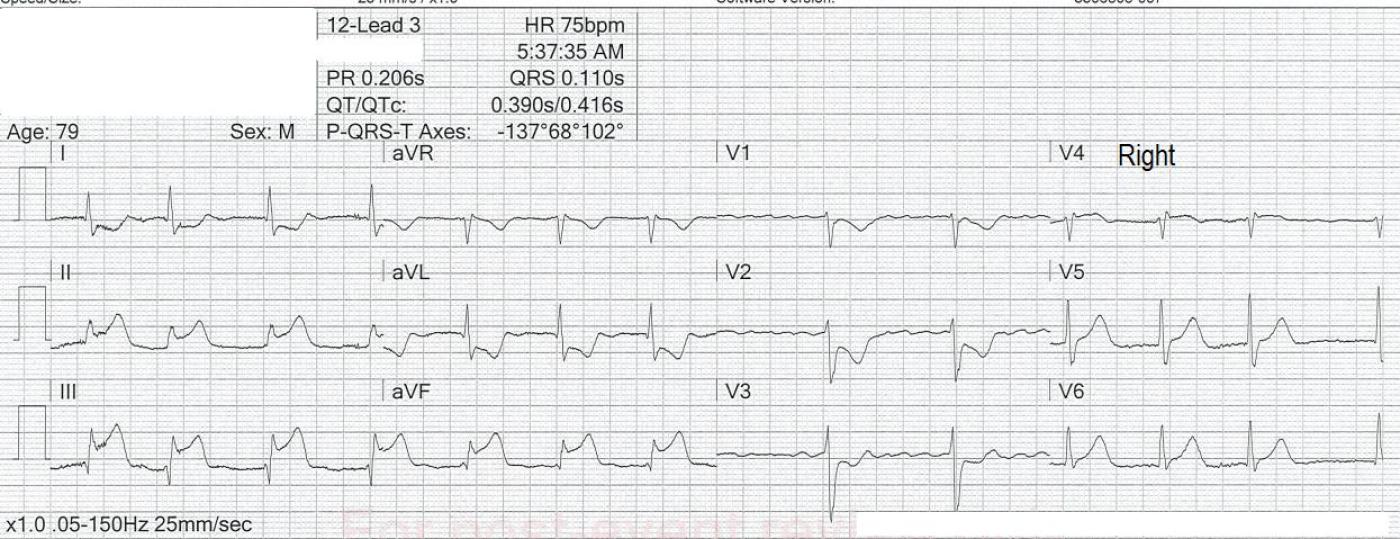
ECG No. 2, obtained at 5:37 a.m., has an additional lead: V4 Right. V4R shows ST elevation, with a flat ST segment and T wave inversion. The right ventricular M.I. has been confirmed. (Note: Posterior wall M.I. could be confirmed with posterior leads, V7, V8, V9. We do not have those here.)
Inferior wall M.I. has a relatively low mortality rate, usually less than 10%. However, the presence of RVMI increases the chance of hypotensive episodes and in-hospital mortality by up to half. RVMI does not change mortality rates after hospital discharge. In addition, the posterior wall extension indicates that this M.I. is a large one, from a proximal occlusion of the RCA.
Summary: Being able to quickly recognize this pattern will help you spot IWMI even before the ST elevations are large. When there is only very subtle ST elevation, the presence of the pattern of STE in the inferior leads and reciprocal STD in aVL make it easy to recognize. Reciprocal STD often shows up before STE, and is more dramatic and easier to spot. When there is also bradycardia, posterior wall M.I., and RVMI, it becomes even easier to diagnose right coronary artery occlusion.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Typical ECG Picture of Acute RCA Occlusion
As per Dawn. Today's tracing presents a typical picture for acute RCA occlusion. I'd add the following thoughts to comments by Dawn.
I agree completely that the ECG picture of acute inferior MI with ST elevation in lead III >> than lead II — with marked mirror-image opposite ST depression in lead aVL (compared to the ST elevation) that we see in lead III — points to the "culprit" artery as almost certainly being the RCA.
In this setting — this ECG is absolutely diagnostic of acute posterior involvement based on the shape and amount of ST depression that is maximal here in lead V2. There is a positive "Mirror Test" (See https://tinyurl.com/KG-Blog-246 — for more on the Mirror Test).
There is NO need to have to confirm posterior lead involvement — because posterior leads in my experience add nothing to what is readily apparent by application of the Mirror Test to a standard ECG. Moreover, because leads placed posteriorly have to pass through the thick back musculature — they typically have much lower voltage, and are more difficult to interpret. In my experience over the years — I have virtually never seen a posterior MI that was evident only on looking at the posterior leads — whereas it is common to see little in the posterior leads in many cases in which the standard 12-lead (via the Mirror Test) is diagnostic. I know many EMS systems routinely advocate for posterior leads — and that is fine. But in my experience, they are not needed once you familiarize yourself with applying the simple Mirror Test (and you can save precious time by not doing them = my opinion).
I emphasized that today's ECG is strongly suggestive of acute RCA occlusion. I was not nearly as sure as Dawn suggests that there was also acute RV involvement. The issue is that when there is acute RV MI — this produces ST elevation in lead V1. But when there is also posterior MI — there is an attenuation of the amount of that lead V1 ST elevation by the posterior MI. It's hard to predict in any given case what the "net" effect on ECG will be.
In general — IF in the presence of acute posterior MI you have a straight or slightly elevated ST segment in lead V1 — then you can be pretty sure that there is also acute RV involvement. However, in my experience — when you have slight J-point ST depressionn in V1 with the shape of T wave inversion that we see in the 1st ECG — this may or may not be "enough attenuation" to reflect acute RV involvement (Remember — acute Posterior MI produces maximal ST depression in V2-to-V4, and not necessarily as much in lead V1). So doing a right-sided lead V4 is indeed advisable to determine if there is or is not acute RV involvement. That said — why ONLY do a single right-sided lead. Better (in my opinion) to do ALL right-sided leads (only takes seconds more once you decide to get any right-sided recording) — and this facilitates what is not always obvious (ie, while lead V4R typically shows the most right-sided ST elevation with acute RV involvement — you'll get a better picture by also recording neighboring right-sided leads).
As to prognosis — MANY factors infuence this. These may include (among others) — age of the patient, prior cardiac damage, state of collateralization, anatomic considerations — site of the MI — but also SIZE of the MI. The marked amount of ST elevation that we see here (with equally marked reciprocal ST depression) suggests a larger MI. And in addition to acute RV involvement — this patient has AFib with a SLOW ventricular response. Especially if this is new AFib — this adds significantly to potential adverse outcome.
P.S. I don't consistently see ST elevation in lateral chest leads in the 1st ECG. Be aware that such lateral chest lead ST elevation is not uncommon with inferior MIs — often the result of posterolateral branches off of the posterior descending coronary artery. Typically with RCA occlusion — the relative amount of ST elevation in lateral chest leads is less than in lead III. I see more of a suggestion of lateral chest lead ST elevation in the 2nd ECG.
That said — this is an EXCELLENT teaching case for what to expect with acute RCA occlusion!
Ken Grauer, MD www.kg-ekgpress.com [email protected]