The patient: Unfortunately, we no longer have information on this patient, other than the fact that she went to the OR for a permanent pacemaker implantation.
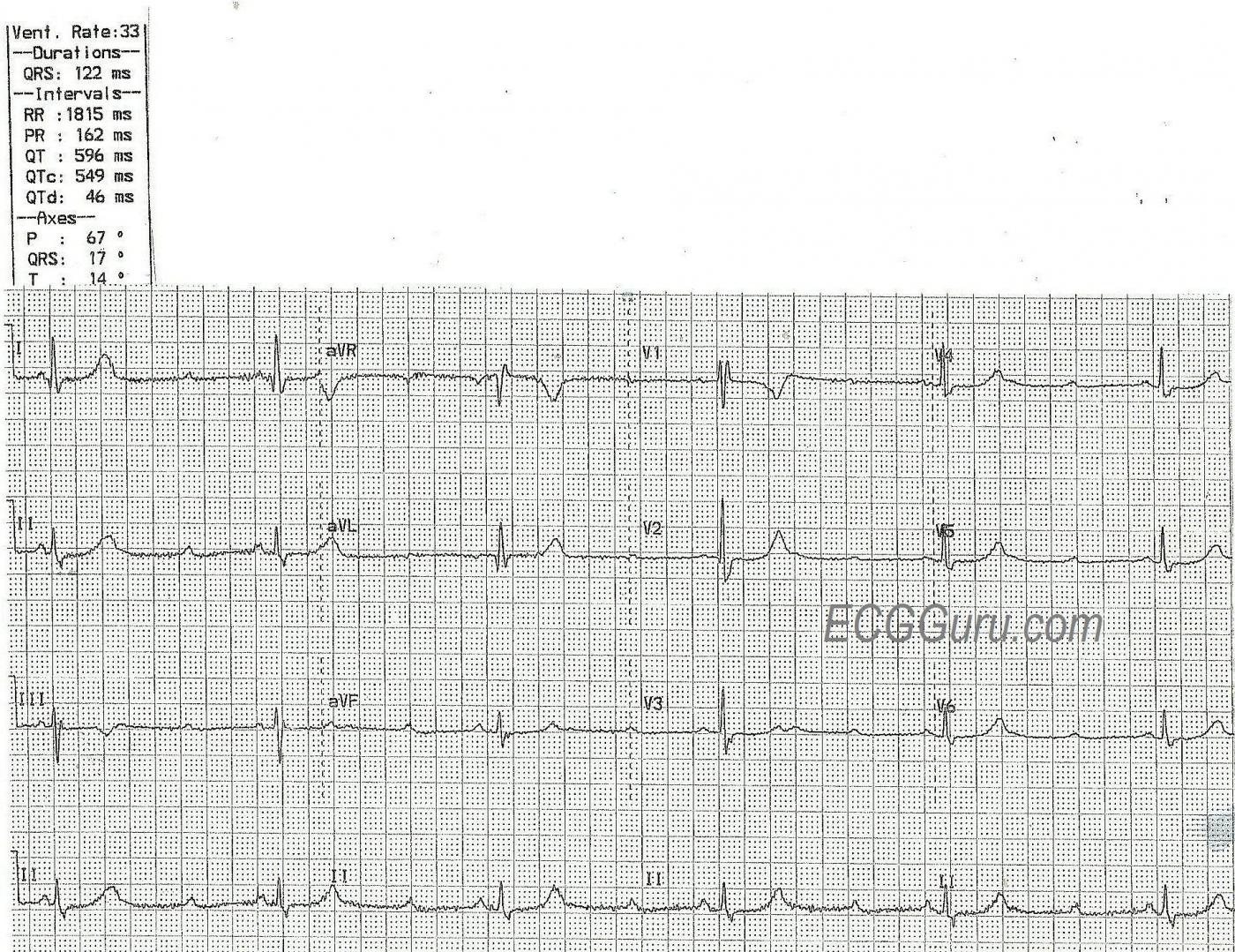
The ECG: The atrial rate (P waves) is 99 beats per minute. The P waves are regular and all alike (NSR). The ventricular rate (QRS complexes) is 33 bpm, and the QRS complexes are regular and all alike. The PR intervals, when A-V conduction occurs, are 162 ms (.16 seconds) and all alike. The QRS complexes are wide, at 122 ms (.12 seconds). There is right bundle branch block, but no left hemiblock, as the frontal plane axis is normal. The QTc is prolonged at 549 ms. Many ST segments on this ECG have a “flat” appearance, rather than the normal concave up shape.
The failure of 2 out of every 3 P waves to conduct indicates a second-degree AV block. Type I is a block of the AV node, with progressive prolongation of the PR interval until ONE P wave fails to conduct. Type II AV block is a block of the intraventricular conduction system. Clues that a second-degree AV block is Type II include:
· The PR intervals are all alike.
· More than one consecutive P wave is not conducted.
· A P wave that is NOT in the refractory period of the preceding beat is not conducted.
· There is evidence of bundle branch (fascicular) block.
This is a second-degree AV block, Type II. Type II blocks are considered to be intermittent tri-fascicular blocks. That is, one or two of the three main fascicles are blocked, and the remaining one or two are intermittently blocked. When conduction proceeds down the working fascicle(s), there is a QRS complex. When the intermittent block occurs, all three fascicles are blocked, producing a temporary complete heart block (trifascicular block). In this example, it appears that the right bundle branch (one fascicle) is consistently blocked, and the left bundle branch (two fascicles) is intermittently blocked.
The most immediate concern for any patient with an AV block is rate. It is important to assess the patient’s perfusion status to determine if the rate is fast enough to maintain BP. Type I AV blocks often respond to atropine, but Type II AV blocks do not, and it may even make them worse. The safest approach is a temporary pacemaker, either transcutaneous or transvenous, to stabilize the patient. Type II AV blocks usually require a permanent implanted pacemaker, as they tend to worsen and lead to third-degree AV block with ventricular escape (rate < 40 bpm) or ventricular standstill.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
AV Block: Probable Mobitz II
Today’s ECG is an excellent case for discussion that highlights distinction between the types of 2nd-degree AV block. In the hope of stimulating discussion — I’ll add the following points to Dawn’s excellent description, emphasizing that many of the points I will make are advanced, and extend “beyond the core" of basic knowledge:
Semantics enter into the classification of AV conduction disorders. As a result of a 2009 AHA/ACCF/HRS Consensus Statement — the term “Trifascicular Block” is no longer recommended — because of potential significant variation in anatomy and pathology associated with this condition. Instead — confusion is best avoided by specifying each conduction system disorder that is present. In today’s case — this entails RBBB (Right Bundle Branch Block) and 2nd-degree AV Block with 3:1 AV conduction, in which the ventricular rate is ~35/minute.
The 2nd-degree AV blocks are divided into 3 Types: i) Mobitz I ( = AV Wenckebach) — in which the PR interval progressively increases until a P wave is non-conducted — before the cycle resumes again; ii) Mobitz II — in which the PR interval remains constant, and one or more P waves are non-conducted; and, iii) An indeterminate form of 2nd-degree AV block — in which it is impossible to tell for certain from a single tracing if the conduction defect is Mobitz I or Mobitz II. Most often — there is 2:1 AV block with this indeterminate form, but it is possible (albeit unusual) for there to be 3:1 AV block in a Wenckebach conduction disturbance.
NOTE: Since we never see 2 conducted P waves in a row in today’s tracing — it is impossible to know IF the PR interval would increase if given a chance to do so. As a result — technically speaking, we can not rule out the possibility of Mobitz I 2nd-degree AV block for today’s tracing, because there is consistent 3:1 AV conduction without ever seeing 2 conducted P waves in a row.
That said, as per Dawn — the Mobitz II form of 2nd-degree AV Block is more likely than Mobitz I in today’s case because: i) The QRS complex is wide (due to the underlying RBBB); and, ii) Consecutive P waves are consistently non-conducted.
Clinically — much more important than the semantics of whether the conduction disturbance in today’s case represents Mobitz I or Mobitz II, is the fact that there is additional conduction system disease (ie, RBBB) — and regardless of whether today’s tracing represents Mobitz I or Mobitz II 2nd-degree AV Block — there is evidence of high-grade AV block with consecutive non-conducted P waves that results in a markedly bradycardic rate of ~35/minute. Unless a reversible cause of these conduction defects is quickly found — the chances are great that a pacemaker will be needed.
Otherwise, a number of additional subtle ECG findings are seen on today’s tracing:
— A fairly deep Q wave is seen in lead aVL. This clearly is deeper than one expects for a simple “septal” Q wave in this lateral lead — so this Q wave in lead aVL may indicate prior infarction at some point in time.
— A small-but-definite Q wave is also seen in the single QRS complex present in lead V2. Such a Q wave is not an expected component of RBBB — so it may also be a marker of prior infarction.
— ST-T waves are uncharacteristically straight in multiple leads. Several leads may show slight ST depression (ie, leads II, V4,V5,V6). The T wave inversion in leads III and V1 is not necessarily abnormal as an isolated finding (both may be a result of the RBBB) — but the T waves in leads I, aVL and V2 are clearly taller-than-expected, as well as being more “voluminous” than expected (wider at their base). There may be slight ST elevation in lead aVR. NOTE: All of these findings are subtle (!!!) — and more difficult to assess since the very slow ventricular rate limits the number of QRS complexes in each lead. That said, in combination and in association with the above-noted conduction defects — these are potentially significant ST-T wave findings.
— Finally, Did YOU see the 2 “little humps” in lead V3? The 2nd of these little “humps” is neither P wave nor T wave — but rather a U wave. To determine this — one correlates the timing of this 2nd little “hump” with the timing of known P waves in the simultaneously-recorded long lead II rhythm strip at the bottom of the tracing. If you look closely — you’ll also see a tiny, terminal little “hump” fusing with the very end of the T waves in leads V2, V4 and V5. That said, in addition to hypokalemia — both LVH and bradycardia are often associated with U waves, so this finding is not necessarily of clinical significance (even though it is a finding that the astute ECG interpreter should recognize).
BOTTOM Line: Today’s tracing shows sinus rhythm — high-grade 2nd-degree AV Block with 3:1 AV conduction and marked bradycardia at ~35/minute — underlying RBBB — subtle Q waves possibly indicative of prior infarction — and subtle-but-real nonspecific ST-T wave abnormalities in multiple leads that really do not localize, and which do not appear to be acute — BUT which do suggest to me the likelihood of significant underlying coronary disease (possibly multivessel, and possibly the result of a fairly recent event) that is the probable cause of the severe conduction defects that we see. I suspect this patient ended up with a permanent pacemaker. Unfortunately, no follow-up is available ...
P.S. For those interested in more on the Basics of AV Block — Please CLICK HERE for my 1 hour ECG video on this topic. If you click on SHOW MORE on the YouTube page (below the video) — you’ll find a linked Contents to all in the video that allows rapid access to whatever section you are looking for.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Terminology
I agree entirely with Dawn’s and Ken’s analysis and interpretation of this ECG but the plethora of different terminologies for describing AV block, some of them used here, can cause confusion. According to the latest (2018) guidance on bradycardias and conduction delays, issued by ACC/AHA/HRS (https://www.ahajournals.org/doi/epub/10.1161/CIR.0000000000000628) this ECG shows an example of high-grade – not second-degree – AV block. The recommendation is that high-grade block should be considered a separate category from – not a sub-group of – second-degree block. I’ve reproduced here the relevant table from the document. Also according to this document, 2:1 block should be considered a separate category from Mobitz I and Mobitz II block. I know that discussion of semantics can be sterile but the complexities of AV block can be so difficult for learners that I do think it may be helpful to standardise on the terminology if that’s possible.
Thank you.
Thanks so much Dave for this important link. For the past forty years of my teaching career, there has been ongoing discussion of the "AV block" nomenclature, with nearly everyone agreeing that the old system of degrees is very inadequate. All attempts to make permanent changes have failed to filter down to the "beginner" level. First, the topic of conduction delay and failure is such a complicated one, it can quickly overwhelm the beginner. Also, the internet is full of entertaining ways to differentiate the blocks, using music, rhymes, analogies, and costumes. Nearly all are inaccurate. So, they remain in the basic texts as they have been for 100 years. I have been hoping "high-grade AV block" would at least gain a foot hold at the basic level, but I accidentally left it off the initial discussion above. I would be ever so happy to publish an article on this site's "Ask the Expert" area that outlines a simple way to explain the AV blocks at a level a beginner monitor tech can understand. It would be very helpful to instructors who have students who do not have extensive A&P and clinical backgrounds.
And, when we accomplish the simplification of conduction blocks for beginners, maybe we can tackle "SVT". :-D
Thanks again for your very helpful comments and link. So appreciated. And thank you, Dr Grauer, for your contribution as well.
Dawn Altman, Admin
New Classification of AV Block
THANKS so much for your comment Dave! GREAT article you cite — and the ePub version (highly recommended!) at the link you give adds a linked Table of Contents, and facilitates seeing the references. AMAZING work in this Consensus Guideline!
I’m adding a Table (attached) that the Authors place at the beginning of their Consensus Guidelines on 10 “Take-Home” Messages for the Management of Bradycardia and Conduction Disorders. These include PEARLS of wisdom that I’ve gleaned over the years — but which are not “officially” cited. Unfortunately (in my opinion) — the language of these 10 Messages is not simple … (ie, written for the cardiology community with extreme care to be “correct” in all ways … ) — but the Messages ARE important. For example — SSS may “go away” after you diagnose and treat sleep apnea (which is so often forgotten as a possible cause of the most worrisome bradyarrhythmias).
Equally important is specific suggestion to NO longer require a specific “pause duration” (which typically used to be ≥3.0 second) before considering permanent pacing with SSS. I was frustrated by previous recommendations that for years in patients who I KNEW were going to ultimately get a pacemaker if they could just stay alive “long enough”, despite their severe Sick Sinus Syndrome that did not yet produce pauses of ≥3.0 second that were captured on a monitor …
As to the new classification of AV block (that you attached) — it conveys important messages — but also potential confusion (in my opinion). Vagally mediated AV block IS clearly a different entity (with different prognosis and treatment implications). This entity is not common — but very important to recognize when it does occur. First degree AV block is not truly a “block” — although I’m less certain that removing it from the “3 degrees” of AV block is beneficial (because of how common 1st-degree AV block is associated with 2nd-degree Mobitz I AV block …).
Finally — I believe it truly is “semantics” to separate out “high-grade” AV block from a type of “2nd-degree” AV block — and in my opinion, it is NOT necessarily helpful to do so. High-grade AV block (ie, non-conduction of 2 or more consecutive P waves that SHOULD conduct but don’t) is often a part of a 2nd-degree AV block. For years I’ve simply said, “high-grade” 2nd-degree AV block” as my diagnosis, adding specification of atrial and ventricular rates and duration of any pauses — and I think doing so most clearly conveys the nature of the conduction disturbance in front of you. I don’t think an “all or none” approach (ie, it’s either 2nd-degree AV block or “high-grade” AV block) serves the best purpose for the multitude of non-cardiologist providers charged with evaluating these patients.
THANKS again for your comment Dave! LOTS of information is contained in this incredibly detailed Consensus Statement that does clarify numerous important issues!
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Terminology
Thanks, Ken and Dawn, for your comments. have no strong feelings about how AV block should be classified but because, although officially retired now, I still occasionally teach ECGs on undergraduate and postgraduate courses I feel obliged to teach to authoritative and influential guidelines wherever possible. In my experience AV block causes more confusion than any other subject in electrocardiography. There are many reasons for this, I think, including the different classification systems and nomenclatures, poor explanations in some textbooks, oversimplification by some teachers (easy learning tends to be at the cost of true understanding) and the fact that some of it is genuinely difficult. So, to teach a difficult subject, it may be helpful if we can at least all standardise on a particular classification scheme whilst acknowledging that these things do evolve as new information emerges. I’ll desist from engaging in a full-scale rant but even the most basic terminology we use in describing AV block is often illogical or misleading. Take 3:1 block, for instance. It means that 1 in 3 atrial impulses conducts, so why not call it ‘1-in-3’ conduction or, if we wish to convey the idea of block, describe it as ‘2-in-3 block’? And to add to the confusion, Ken described the ECG under discussion as showing 3:1 conduction, by which he meant that 1 in 3 atrial impulses conducted. But he also talked about 3:1 block! This is certainly not a criticism of Ken, but AV block is something that many of us are very comfortable with, and this enables us to cope quite easily with unclear or ambiguous nomenclature that can be puzzling to the new learner. I think we need try to get into the head of the learner and attempt to see things from their point of view. There are many other examples I could quote but I’ll leave it there!
A Parting Look at "Terminology"
Always fun, interesting and educational discussing issues with you Dave! That said — I fear the issue of terminology is not one that will be decided by the 2018 Consensus Statement that you cite above (although this truly IS an excellent, thoroughly referenced work!). And I agree entirely with you that it would clearly help to have a single, authoritative source to model our terminology after. Unfortunately — the Table you reference (as helpful as it is in citing the major types of AV conduction disturbances) — is problematic in a number of ways. These include:
i) Specification of a PR interval of >200 ms as constituting “atrioventricular delay” — when in fact, a PR interval of 0.21-0.22 second can be a normal phenomenon reflecting increasing vagal tone as a result of athletic endurance training.
ii) Specification of a regular atrial rate of less than 100/minute for determination of Mobitz I and Mobitz II forms of AV block — when sinus arrhythmia and ventriculophasic arrhythmias are common accompaniments of AV block. And this leaves us with the question of how to define clear 2nd-degree AV block when the atrial rate is faster than 100 (say ~110/minute).
iii) What to do with clear evidence of Mobitz I in which there are 2 consecutive P waves that “do not conduct with evidence for some atrioventricular conduction” for the simple reason that junctional escape occurred before this (ie, so we have no idea if there might be some atrioventricular conduction if there wasn’t that junctional escape).
iv) Missing the KEY requirements of 3rd-degree (complete) AV block — which are that you MUST see P waves in ALL phases of the cardiac cycle to ensure that there truly is NO evidence of AV conduction DESPITE having adequate opportunity to conduct. Simply saying “No evidence of AV conduction” (as their Guidelines do) is the reason I’ve seen too-numerous-to-count examples over the years of interpreters saying “3rd-degree AV block” without being aware of the need to establish that there was indeed no conduction despite adequate opportunity to conduct.
v) Lack of defining how “mediation by heightened parasympathetic tone” is determined.
vi) How does adding “Infranodal block” add to this classifcation beyond clear evidence of Mobitz II?
I realize the “points that I pick” above could be considered too highly detailed — but I simply feel we are not yet “there” with Consensus Guidelines for an acceptable, all-inclusive classification. I realize others may disagree with me — and that is fine.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
AV Blocks - Probably the WORST Defined ECG Terminology
The only definition worse than AV blocks is the distinction between a sinus pause and a sinus arrest.
I agree with everyone that there is a conundrum of definitions and myths regarding AV blocks, such as...
1. First degree AV blocks are all benign and do not require treatment or futher investigation. WRONG!
2. Mobitz I involves a gradually increasing PR interval and then a QRS is dropped. WRONG! and WRONG! The PR intervals may not increase progressively during an atypical Mobitz I (and we now know that most sequences are atypical) and, though there will be a final P wave in the sequence that fails to conduct, one should not involve "dropped" QRS complexes in this definition since a junctional escape beat may provide a QRS after the non-conducted P wave, leaving a QRS for every P wave in the sequence.
3. A cardiology fellow preparing for her boards took my advanced course. She had brought along a book on electrocardiography recommended to her by her cardiology department. The definition of 3rd degree AV block in that book was: "P waves and QRS complexes that bear no relation to each other." That was it - nothing more to the definition! My assessment? An electrocardiography book bearing no relation to fact!
My thanks to Dawn, Ken and Dave for an excellent discussion.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
I decided to revisit this ECG
I decided to revisit this ECG and in doing so, I noticed something - even when I enlarge the tracing, I still feel that the QRS complexes are slightly less than 0.12 sec in duration. That is simply not compatible with any Mobitz II AV block that I've ever seen or even heard about. It makes me wonder if the P wave hidden in the T wave concealed as far as the lower AV node and left it too refractory for the next P wave to pass through after being blocked in the upper AV node. By the time the next P wave arrived, the AV node had recovered enough to conduct normally. I suppose it is possible that the block may be in the distal His bundle, but my understanding is that such a block would be extremely rare.
What do you think?
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
Interesting point
Dr.Jones,
Thank you for another thought-provoking take on this ECG. I see the point you are making. I'm not sure I agree with the QRS width being below .12 seconds. This is a photocopy, and the paper has "dots", rather than lines, for the small blocks. Using an online caliper for my computer, I got just at .12 sec. Assuming the QRS is narrow, I suppose a distal His block could be the culprit, or prolonged refractory periods due to the first non-conducted P waves. What I don't know is how much delay could actually occur from this type of concealed conduction? It has always been my opinion that a P wave "out in the middle of nowhere" that does not conduct has to have a very compelling reason for not conducting, usually "Type II" AVB But, if you are correct that the QRS is narrow, that does change the possibilities I'm still going with RBBB, with poor photocopy quality and RBBB pattern as my justification.
. In my former clinical practice, my only consideration in the moment would be whether the patient needed support for the slow rate. (This patient ended up with a permanent pacemaker). In my later years of clinical nursing, I was fortunate to work in a full-service cardiac hospital with an excellent electrophysiology lab and amazing electrophysiologists. I was surprised (or dismayed?) at how often my ECG interpretation was not exactly what was found in the EP lab. And I was inordinately giddy when they demonstrated that I was right all along! Good times.
Dawn Altman, Admin
Thanks!
I certainly agree with you that while the P waves and the failure to conduct create quite a conundrum for the interpreter, it's the QRS complexes that are important for the patient. I enlarged one the of QRS intervals from V1 to illustrate. If it's nothing more than a poor enlargement - then no big deal. If the ventricular depolarizations are indeed < 0.12 sec, then this is a very remarkable tracing!
Jerry
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
I see your point!
Yes, I definitely see your point, Jerry. Maybe I own a very rare ECG! At the very least, it provided a lot of interesting conversation, and some good thought exercise. Wish we had an EP study.
Dawn Altman, Admin