The Patient A 64-year-old woman has called 911 because she has chest discomfort radiating to her left arm, palpitations, weakness, and a headache. She had a valve replacement (we do not know which valve) two weeks ago and has a healing incision over her sternum. She is found sitting in a chair, pale, cool, and diaphoretic. Her blood pressure is 94/palp. Her pulse rate is 196 bpm and weak. She is afebrile.
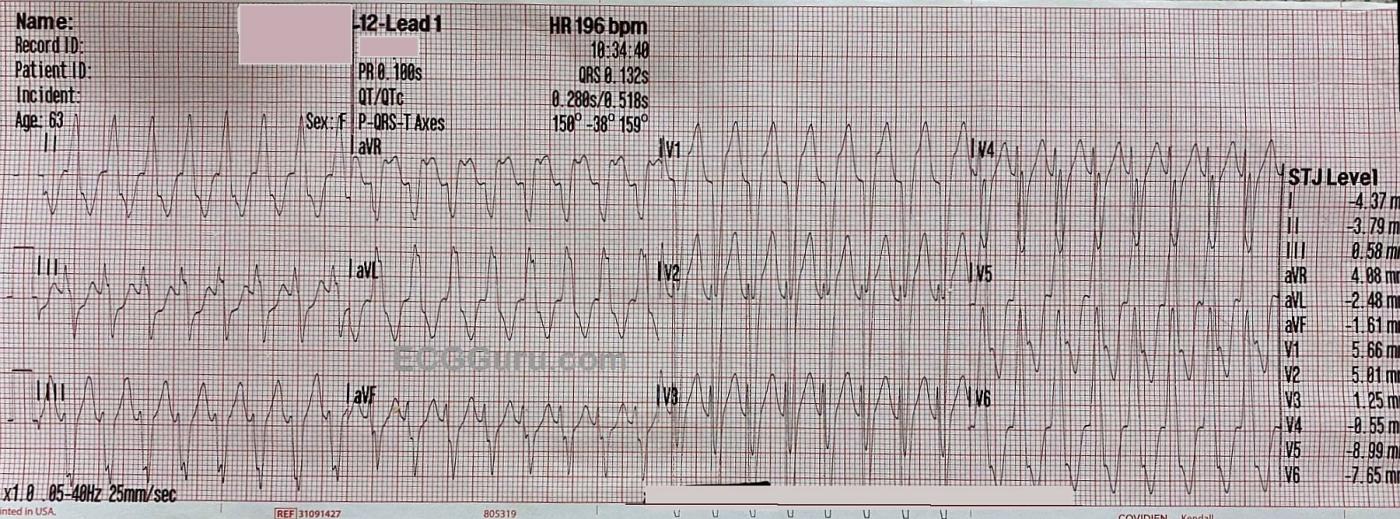
ECG #1 This ECG shows a wide-complex tachycardia at 196 bpm. The QRS complexes are .132 seconds in duration, per the ECG machine. The rate is too fast to appreciate whether there are P waves present. We did not see the onset of the tachycardia, but with a rate this fast and regular, it is most likely a reentrant rhythm, rather than sinus tachycardia. An abrupt onset of the rhythm would point to a diagnosis of a reentrant rhythm, either ventricular tachycardia (VT) or paroxysmal supraventricular tachycardia (PSVT).
There is an important rule in emergency medical care: a wide-complex tachycardia should be treated as VT until and unless it is proven to be something else. The most likely alternate interpretation is PSVT with aberrant conduction, which usually takes the form of left or right bundle branch block. Fortunately, the paramedics on this call have a protocol for treating WCT that includes electrical cardioversion for the unstable patient, and amiodarone for the stable patient. This protocol serves both possibilities, VT and PSVT, well. The patient’s perfusion status and BP made her borderline in this determination, but she was alert and oriented, so the paramedics opted for administering the amiodarone while they prepared to electrically cardiovert.
An interesting finding of this ECG is that the pattern for LEFT BUNDLE BRANCH BLOCK is present. The criteria for LBBB is: supraventricular rhythm, wide QRS, negative QRS in V1 and positive QRS in Leads I and V6. Without visible P waves, we cannot prove that this is a supraventricular rhythm, but this looks like LBBB. There are ST changes that we normally associate with LBBB – discordant ST segments. That is, there is ST elevation in leads with negative QRS complexes and ST depression in leads with positive ST segments. For further information regarding evaluating ST segments for M.I. when there are discordant ST changes, I would refer you to Dr. Steven Smith’s, et al, modification of Sgarbossa’s Criteria.
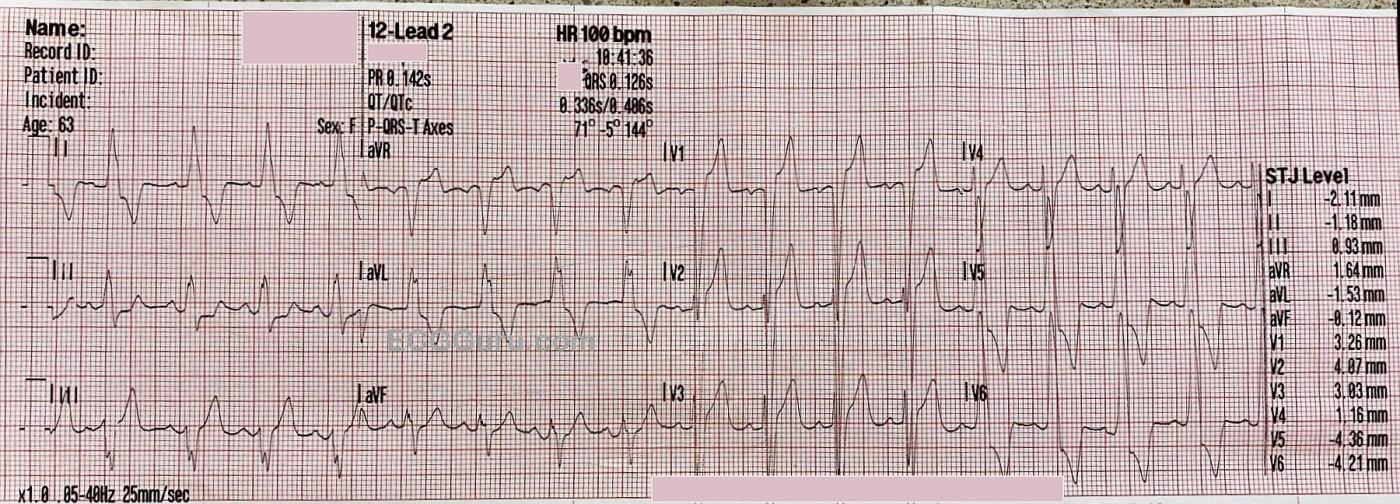
ECG #2 Approximately 7 minutes later, the rhythm converted to sinus rhythm at 100 bpm. When the rate changed, P waves became quite obvious, and the QRS complexes did not change. She now has sinus rhythm with LEFT BUNDLE BRANCH BLOCK, proving that the faster rhythm was also LBBB, rather than VT. She also meets voltage criteria for left ventricular hypertrophy, which causes ST changes similar to those caused by LBBB. At the time of conversion, her BP became 130/P and her skin regained normal color and temperature, without diaphoresis. Her subjective symptoms improved. She was maintained on the Amiodarone drip for the short transport to the hospital. It is possible that this is a rate-dependent bundle branch block, as the sinus rate is around 100 bpm, and the rhythm would need to be reevaluated when she regains a slower rate.
This case is a good endorsement for initial treatment protocols for wide-complex tachycardia that are effective for both VT and PSVT.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
A Regular WCT that Looks Like LBBB
Assessment of the Regular WCT (Wide-Complex Tachycardia) is an essential skill for all emergency care providers to master. This is not to say that it will always be possible to be 100% certain of the diagnosis from the initial ECG. On the contrary — even the most astute ECG interpreter will at times not know a definitive diagnosis at the time that one needs to begin treatment.
The KEY point about today’s case — is that it is OK not to be 100% certain of the rhythm etiology, as long as one remembers: i) If the patient with a regular WCT of uncertain etiology is hemodynamically unstable because of the rapid rate — it no longer matters what the rhythm diagnosis is, because regardless, immediate cardioversion is essential! — ii) IF your patient is stable — then even if the rhythm is VT, you may still have a moment to try medical therapy (knowing that if at any point during the process your patient becomes unstable — that you will then immediately cardiovert); and, iii) Amiodarone is an antiarrhythmic agent that may be effective in treating a variety of both supraventricular rhythms and VT.
I’ve reviewed my step-by-step approach to the regular WCT rhythm of uncertain etiology on a number of occasions. For those interested in review — I suggest the case, from my May 5, 2020 post in Dr. Smith’s ECG Blog — and — my ECG Blog #42.
Regarding today’s ECG Guru case — the patient is a 64-year old woman with recent open-heart surgery for valve replacement. She is described as, “sitting in a chair, pale, cool diaphoretic” with a 94 palp BP and a weak, rapid pulse. Her initial ECG shows a regular WCT rhythm at ~190/minute, without clear sign of atrial activity.
COMMENT: On paper, for a patient this age who is recently post-op for open heart surgery — the above physical description does not sound “hemodynamically stable” (ie, this older patient is hypotensive and symptomatic). Many providers might have immediately cardioverted — instead of trying Amiodarone. That said, “Ya Gotta Be There” — and it turns out that the Amiodarone worked!!! Therefore — one can’t criticize the treatment! But I’ll emphasize that immediate cardioversion would have been equally appropriate.
As per my detailed discussions (at the above-cited links) — We start with an almost 90% likelihood that a regular WCT rhythm without clear sign of atrial activity is likely to be VT. In such cases, it is most prudent to treat the patient as having VT until proven otherwise. That said — as an advanced Point — I’ll highlight that I suspected the initial ECG was going to be one of the ~10% of cases in which the rhythm was an SVT (SupraVentricular Tachycardia) instead of VT!
IF the rhythm in today’s case were to be supraventricular — at a rate of ~190/minute — this would be much faster than is usually seen with sinus tachycardia or 2:1 atrial flutter. Therefore, IF this rhythm was SVT — we would likely be dealing with a reentry SVT rhythm (ie, AVNRT or AVRT).
The reason I strongly suspected this rhythm was not VT — is that it looks completely typical for LBBB because we see: i) Monophasic upright R waves in all 3 lateral leads that I look for ( = leads I, aVL, V6); ii) Not only a predominantly negative QRS complex in at least 3-4 anterior leads — but no more than a very thin initial r wave (seen here in V2, V3, V4) — AND — very rapid S wave downsloping in V1-thru-V3; and, iii) Nothing anywhere that is atypical for LBBB. NOTE: Even with completely typical QRS morphology for LBBB (as we dosee here) — I cannot 100% rule out the possibility of VT — but as an advanced Point — I would have bet ~90% likelihood for SVT, and I probably would have treated this patient assuming a likely reentry SVT rhythm. That said — given her questionable hemodynamic status — I would have been ever ready to cardiovert if she showed any sign of deterioration. I WILL REPEAT — I would fault NO ONE for assuming VT and treating accordingly. But the more advanced interpreter might well suspect an SVT ....
The Post-Conversion ECG — It’s always nice when our treatment works, and we now see conversion to sinus rhythm. Note there still is LBBB — with an identical morphology as during the initial WCT rhythm! This confirms the SVT etiology of the initial rhythm. Very deep anterior S waves (>25-30 mm) indicate LVH (despite the presence of LBBB). There still are ST-T wave changes (depression and elevation) — but these are lessthan during the WCT rhythm, and probably not indicative of acute ischemia given the recent persistent tachycardia and the LBBB with such huge QRS amplitudes.
Ken Grauer, MD www.kg-ekgpress.com [email protected]