This ECG was taken from a 78-year-old man who was experiencing chest pressure in the morning, after having left shoulder pain since the night before. He has a history of hypertension and hypercholesterolemia, and has an implanted pacemaker.
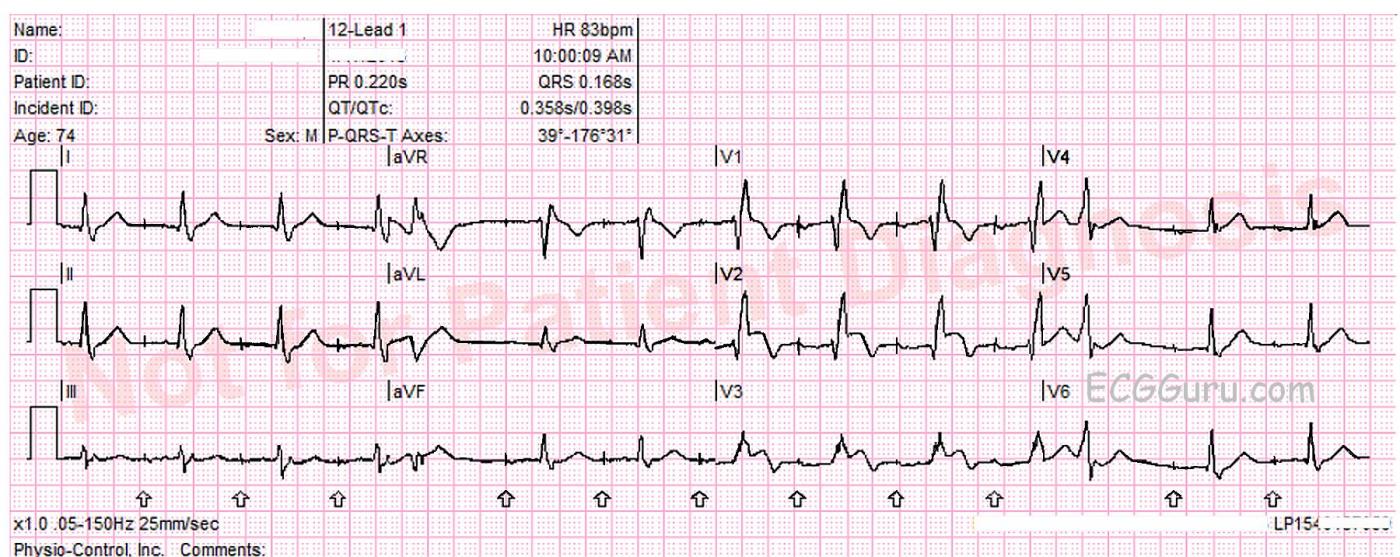
What does the ECG show? The ECG shows an atrial paced rhythm, with two premature beats, beats number 5 and 12. These are probably PVCs. The patient has a functioning AV conduction system, so the paced atrial beats are conducting through the AV node and producing QRS complexes. In the interventricular conduction system, the impulse encounters right bundle branch block. This causes each QRS to have an “extra” wave attached at the end, representing slightly delayed depolarization of the right ventricle. Instead of an “rS” pattern in V1, for example, we see “rSR’ “. The slight delay causes the QRS to be widened, as we are measuring the two ventricles separately, rather than synchronously.
There is definite ST segment elevation in V2 and V3, and the shape of the ST segment is straight, having lost it’s normal “concave upward” appearance. In an ECG taken three minutes later, the STE extends to V4.
Do the pacemaker or the right bundle branch block prevent us from diagnosing an ST-elevation M.I.? The answer to that is a resounding “NO!” Pacemakers can sometimes make it difficult to assess ST elevation because ventricular pacing causes ST segment changes. Pacing the right ventricle causes a depolarization delay in the left ventricle as the impulse travels “cell to cell” across the LV. This means an RV-paced beat will resemble a PVC from the RV. When LV depolarization is altered, repolarization will also be altered, causing ST elevation in leads with negative QRS complexes, and ST depression is leads with upright QRSs. These are called discordant ST changes. These changes are proportionate to the height or depth of the QRS, with very minimal or no ST changes in leads with short or biphasic QRS complexes. We don’t have to worry about that in this situation – the pacemaker is not pacing the ventricles.
You might have heard that bundle branch block makes it hard or even impossible to diagnose STEMI. Left bundle branch block can cause some difficulty because, in LBBB, the left ventricle is depolarized via the right ventricle, instead of via the left bundle branch. Like in RV pacing, the slow, cell-to-cell depolarization that results from LBBB also causes ST changes that are discordant to the QRS complexes, and proportionate to the size of the QRSs.
But this patient has right bundle branch block. The left ventricle is depolarizing (and repolarizing) normally, while the conduction delay is in the right ventricle. Since the M.I. is in the left ventricle, these obvious ST elevations indicate acute STEMI.
Patient outcome. The EMS crew called the hospital with a “STEMI Alert”. A second ECG showed increasing STE. The patient’s troponin level was 0.33 ng/mL in the Emergency Dept. (Normal troponin is less than 0.01 ng/mL). He was rushed to the cath lab, where an occlusion was found in his left anterior descending artery. The artery was opened and stented successfully.
Thanks to Lew Steinberg, Ryan Winkelman, and Palm Beach Gardens Fire Rescue for this interesting tracing.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Atrial Pacing + Acute STEMI ...
I agree completely with Dawns interpretation. There is atrial pacing — but very typical RBBB conduction (sharp rSR’ complex in V1; wide terminal S waves in leads I, V6). There should be NO DOUBT in a patient with new chest pain that there is acute anterior STEMI ongoing — with hyperacute ST elevation + beginning T inversion in leads V2,V3 (and lesser changes in a number of other leads).
P.S. Atrial pacing spikes are easily seen on this tracing. I had to look "long and hard" to try to determine if there was ventricular pacing — because there is a LOT of baseline artifact! The reason I believe there is no ventricular pacing — is how "clean" and absolutely typical QRS morphology is for complete RBBB — and that wouldn't be seen if the ventricles were being paced ... As per Dawn, it is often much more difficult (if not impossible) to detect very subtle acute ischemic ECG changes on paced tracings — but sometimes you most definitely CAN detect acute stemi when there is obvious ST elevation that just shouldn't be there ... But in tracings like this in which there is atrial but not ventricular pacing — then you simply have RBBB, and (as per Dawn) — much (if not most) of the time with RBBB you WILL be able to detect fairly subtle acute ischemic changes. And when the ST elevation is marked and as abnormal as it is here — there should be little doublt of acute STEMI in progress.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Excellent Case, Dawn!
I wrote a similar comment earlier but I don't think it actually got posted.
I also agree with you 100%. Not only should a STEMI be readily detectable in RBBB, STEMIs are USUALLY readily detectable in LBBB as well. Most of the confusion arises when when V1 - V3 are involved. I still encounter people who refuse to commit themselves to a diagnosis of STEMI in the presence of LBBB even when the STEMI is OBVIOUS!
I do have concerns about the pacemaker, however. Like Ken, I spent time trying to find a ventricular pacemaker artifact and could not find one. However, that doesn't rule out sensing in the ventricle. Fortunately, there is a PVC to help us with that. If there were ventricular sensing occurring, the right ventricular lead would have sensed it and then inhibited the atrial pace. Well, I don't see any atrial pacing artifact occurring exactly where one would expect (at the end of the atrial lower rate limit), so there is no atrial pacing spike. Was it indeed inhibited? If so, the point at which the ventricular lead sensed the PVC would be the starting point for another atrial pacing interval. To find the point at which the PVC was sensed, we measure back one atrial pacing interal (lower limit interval) from the pacin spike following the PVC. When we do so, we see that the PVC would have to have been sensed virtually before it was initiated. Ventricular wires usually take much longer to sense a PVC (often 40 msec or more) and initiate another atrial pacing interval. Something just insn't adding up here. My only explanation at this point is that the PVC is probably a bit wider than it looks and was actually initiated sooner after the conducted QRS than it looks. Any ideas?
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd