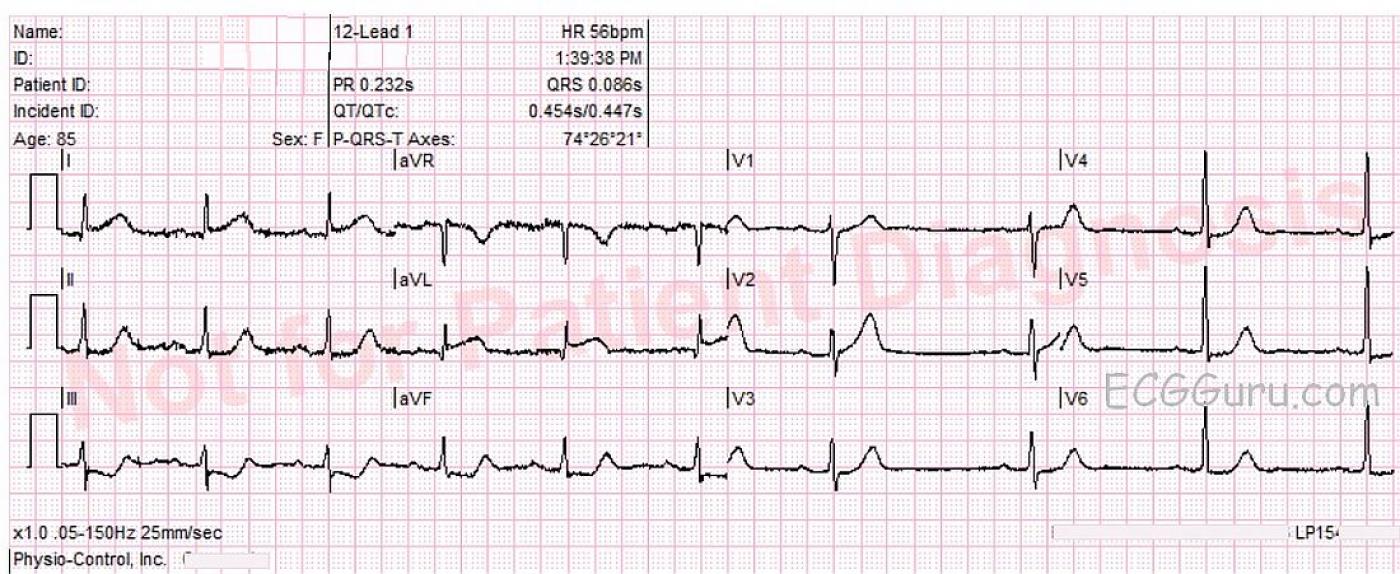
This ECG is taken from an elderly woman with chest pressure radiating to left shoulder for 30 minutes. She also complained of nausea with vomiting. Her family offered a history of unspecified cardiac disease, hypertension, hypercholesterolemia, and dementia.
The ECG shows ST elevation in Leads I and aVL, with reciprocal ST depression in Leads III and aVF. ST segments have an abnormally flat shape in Leads aVL, II, III, aVF, V5 and V6.
She was admitted to the hospital and sent to the cath lab. Her arteries were found to be clear, and Takotsubo cardiomyopathy was diagnosed. See also.
Our thanks to Lew Steinberg and Palm Beach Gardens Fire Rescue for donating this interesting ECG.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
An Elderly Woman with Takotsubo ...
Interesting case from an elder woman with chest pressure! Unfortunately, a long lead rhythm strip is missing. That said, the rhythm appears to be a marked sinus arrhythmia with 1st-degree AV block (PR interval ~0.22 second). The axis is normal — the QRS and QT intervals are normal — and there is no chamber enlargement. The most remarkable findings are coved (hyperacute) ST elevation in both high lateral leads (leads I, aVL) — with a hyperacute ST-T wave in lead V2 (and perhaps to a lesser extent in V3, V4). Other leads show ST-T wave flattening, with a picture of “mirror-image” ST depression in lead III with respect to the ST elevation with see in lead aVL. The picture looks like an acute STEMI ( = ST Elevation Myocardial Infarction) — although determination of the “culprit artery” is a bit more challenging. One usually expects lateral chest lead ST elevation with LCx (Left CircumfleX) occlusion. The 1st Diagonal branch of the LAD (Left Anterior Descending) artery typically supplies the high lateral wall, and occlusion of this 1st Diagonal branch may provide a picture of ST elevation in lead aVL and in lead V2, but in no other anterior leads. That would have been my guess for the “culprit artery” in this case. Alas, we are told that cath showed clean coronary arteries, with a picture consistent with Takotsubo Cardiomyopathy.
Comment: This is why cardiac catheterization is done. It keeps us “honest”. Even when one thinks the answer is known — there will be occasional surprises. That said, correct management was pursued in this case. It was recognized that prompt cath to define the anatomy was indicated — and doing so confirmed that this ECG picture in this patient was not the result of a STEMI.
Brief review of Takotsubo Cardiomyopathy can be found HERE. To my knowledge, there is no diagnostic ECG picture. Instead, a variety of ECG findings may be seen. The diagnosis can be suspected in elderly patients (especially female) when a clear history of preceding physical or emotional stress can be elicited. Heart failure is common. Usually there is no more than modest troponin elevation. In my experience — the ECG picture often “does not fit” the distribution for that of a typical STEMI … — but not uncommonly, cath will be needed to make the diagnosis. The “good news” is that these patients generally have a favorable longterm prognosis — often with full recovery over ensuing weeks (but occasional fatalities may occur).
Ken Grauer, MD www.kg-ekgpress.com [email protected]
...
Great comments! As we both know, stress cardiomyopathy can present with almost any injury pattern on the ECG, but I have to wonder...
Most often, SCM presents with an anero-apical or "global" injury pattern. Since this is an atypical injury patten, and since ostial diagonal artery occlusions are occasionally invisble on cath (see this case that we've discussed before: https://www.facebook.com/groups/ekgclub/permalink/506431559439853/), I'd be interested in seeing just how they confirmed the diagnosis of SCM. Was there true ballooning of the apex circumferentially? Or was it a more focal WMA affecting the anterolateral territories?
With increased recognition of SCM and increased awareness of its spectrum of variants, we run the risk of widening our net too much and calling something an "atypical SCM" when it's really a missed but typical STEMI.
Obviously we can't say anything definitive here and have to (provisionally) accept the diagnoses made in the hospital, but I just wanted to throw that idea out there.
Vince D
http://www.medialapproach.com
A rather atypical Tako-Tsubo
While recognizing that Tako-Tsubo can present with various ECG findings, the present ECG looks rather atypical to me in comparison to "classical " appearance of Tako-Tsubo syndrome: though neither absolutely definitive nor diagnostic, I would have expcted more prolonged QTc and especially ST elevation in inferior leads (in accordance with the peculiar myocardial involvement. Anyway, as we all know the diagnosis should be confirmed on echo or ventriculography (apical balooning) or at worst by observing improvement of EF over time.
Mario Parrinello
Agree with above comments
Thank you all for your comments. I agree that this is an atypical ECG pattern for the diagnosis. This was given to me with the hospital's diagnosis, and I did not see the patient or the cath procedure. I will try to find out more.
Dawn Altman, Admin