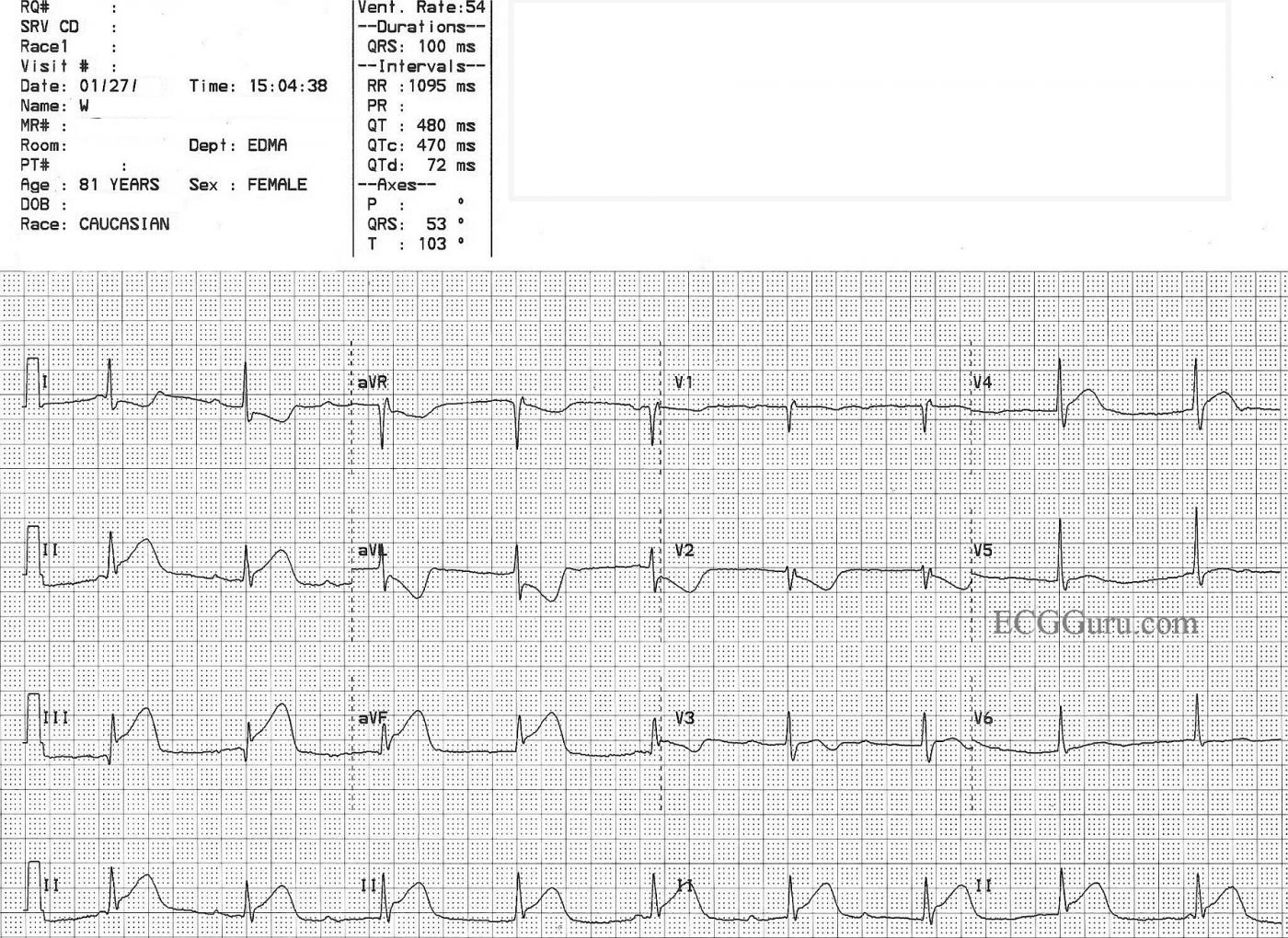
We do not have a patient history for this ECG, other than that it was an 81-year-old woman with chest pain. The classic signs of acute ST-elevation inferior wall M.I. are there: ST segment elevations in Leads II, III, and aVF. There are the expected reciprocal ST depressions in Leads I and aVL. The ST depression in V2 suggests posterior wall injury, and would normally be seen in V1 as well, unless something else is causing ST elevation in V1 at the same time. That "something" would be right ventricular injury, and it can be confirmed by performing a V4Rt (or full set of right-sided V leads). The slight elevation in V3 and V4 don't seem to "fit" with the IWMI - one might expect V5 and V6 to have ST elevation, reflecting injury in the low lateral wall. We don't have the cath lab results, so we do not have an explanation for this (lead placement issues, perhaps?).
The rhythm here is interesting, but not unexpected with IWMI. The rhythm is junctional, as reflected by the regular, narrow QRS complexes at a rate of about 54/min. IWMI often causes blocks of the AV node, which has the same blood supply as the inferior wall in most people. Even though there appear to be some "PR intervals", they are not consistent, and also do not meet the criteria for second-degree AVB Type I, so we are left with an interpretation of complete heart block. The P waves here are also inconsistent. They are regular at times, then disappear. The SA node can be affected in IWMI also, and develop rate irregularities and exit blocks. The IMPORTANT thing to consider is how the patient is handling the rate. If this rate is not causing perfusion problems, that is - the patient has enough rate to maintain her blood pressure and level of consciousness, the rate is not harmful, and the junctional rhythm is not harmful. In fact, one could argue that this junctional rhythm is more beneficial to the injured heart than a faster sinus rate would be.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Acute RCA Occlusion with Complete AV Block
Looks like infer-postero and RV MI from acute proximal RCA occlusion. ST elev in lead III > II with marked ST dep in aVL supporting RCA occlusion - with pos “Mirror Test” in lead V2 supporting acute post MI (and also note disproportionately tall R wave abruptly appears in V3 - which is consistent with post MI). Lead V1 actually seems to show some ST elev (but at the least a coved ST segment) - which in context with the marked ST dep in V2 is enough to strongly suggest acute RV involvement.
Progression of ST-T wave changes looks a bit weird in V2-thru-V6 - in that there is ST elevation in V4, but really not in V5, V6 (Were leads normally placed?).
As to the rhythm - I think this is complete AV block with AV nodal escape (P waves completely unrelated to the QRS). The ventricular rhythm has a narrow QRS and is perfectly regular at ~55/minute (consistent with AV escape rate from an acute inf MI). We initially see regular P waves at ~65/minute - then then lose the P waves after beat #3 - and again after beat #7. In addition - the P wave after the pause (ie, the P just before beat #5) is not quite right on time …. nor is the P preceding beat #9 quite on time - almost as if there is some type of high-grade exit block out of the SA node in this patient with obvious large acute ongoing stemi ….
Otherwise - I don’t see PTa deflections that might indicate atrial infarct - and of note that Q waves have already formed in leads III and perhaps in aVF ...
Ken Grauer, MD www.kg-ekgpress.com [email protected]
I left a reply below with my
I left a reply below with my opinion on why there could by ST-elevation in V4. Thoughts? Thanks!
Vince D
http://www.medialapproach.com
Conjecture
If I had to guess, I would suspect the ST-elevation in V4 is due to significant RV MI and not so much a lead placement issue. Typically if there's an error in V4 placement it is because it is too medial or lateral, but the nice R-wave progression across the precordials here suggests that they are reasonably placed. I suppose it could be placed too low and thus "see" the inferior injury vector, but I think it's something else.
There is clearly posterior involvement from the morphology of V2, however the amount of ST-depression in that lead doesn't match nearly how much we would expect with such a large STEMI in II, III, and aVF if it is also affecting the posterior wall. Instead, that expected large ST-depression is attenuated by something, and as Dawn points out, it is because this is a proximal RCA occlusion with RV MI as evidenced by the isoelectric J-point in V1 (which we would also expect to be depressed). V3 should also be showing a large amount of ST-depression from the posterior STEMI - typically it shows the most depression - but here there is actually none. Again, this is caused by a significant RV MI causing an injury vector to "spill over" into the right precordials.
V4 is where the amount of ST-depression from posterior STEMI tends to peter-out a bit, but in this case there is still significantly more RV-ST-elevation at V4 than there is posterior ST-depression, resulting in a net-result of ST-elevation mimicking anterior MI in that lead.
At least that's the story I'm telling myself, but I think it's a good one.
Vince D
http://www.medialapproach.com
Sounds plausible
Hi, Vince,
I was waiting to see if any of the other "Gurus" replied to your comment, but I think they have moved on to other things. Too bad, I wanted to see what they said. I feel, as you do, that the posterior wall is having a great influence on V1, V2, and V3. I am surprised that V4 has a larger elevation than V5 and V6, however, because I am accustomed to seeing IWMI with low lateral elevation due to dominance of the artery. At first, I thought this might be a "V4R", but the QRS doesn't look like it. At least we all agree that it is a STEMI! Thanks for your thought-provoking comment.
Dawn Altman, Admin
cause of junctional rhythm
The rhythm is more likely caused by increased Vagal tone associated with the inferior infarction and not ischemia to the AV node.
Frank Kempf
Cara Mengobati Penyumbatan Pembuluh Darah Di Leher
Great site, I really enjoy your blog. I'm waiting for more. Best regards!
Cara mengobati penyumbatan pembuluh darah di leher
http://www.obatpelancarhaidterbaik.com/
Thanks!
Thank you so much for your comment. We strive to provide quality content. Let us know if you have any special requests. You can email me at [email protected]
Dawn Altman, Admin