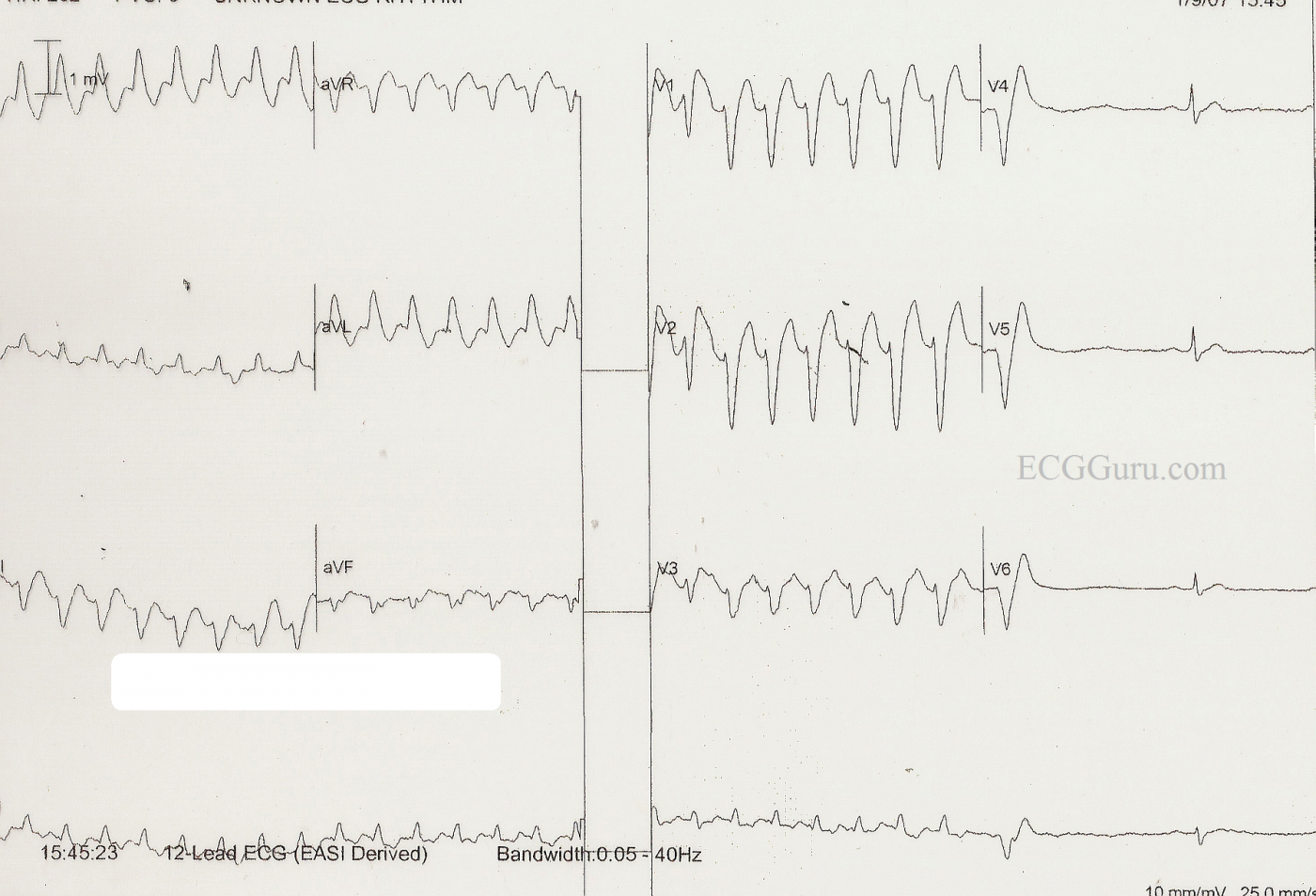
This ECG was presented earlier this week as an example of SVT with LBBB aberrancy, which was ultimately converted with one dose of adenosine in the Emergency Department. It is the most shared and commented on ECG yet to appear on the Guru. The diagnosis given was the one accepted by the medical staff who cared for the patient, who was a man in his 30's who presented to the Emergency Department complaining of a rapid heart rate. He was ambulatory with stable vital signs, in spite of the tachycardia. He reported that he has had several episodes of fast heart rate which responded to either Valsalva maneuvers or, in some cases, medication in the ED. He was told he might benefit from an ablation procedure, but he did not have health insurance and continued to use the ED as his primary source of medical care. When he was admitted to the ED, the tech initially called for help, thinking the monitor showed ventricular tachycardia. The ED physician felt that this represented LBBB aberrancy, possibly rate-dependent, and he treated the patient with adenosine. The rhythm converted to sinus after one dose, and the patient remained stable throughout the process. He was advised to undergo further observation and testing, but he declined due to financial concerns, and the fact that he usually succeeded in relieving his symptoms with "bearing down".
Wide-complex tachycardias can be difficult to assess simply from an ECG. The patient's stability depends more upon general health and cardiac output issues than the origin of the tachycardia. When we presented this ECG, we also presented the diagnosis he had upon discharge from the ED.
Subsequently, ECG Guru Dr. Ken Grauer, a frequent contributer to this site, offered his alternative diagnosis and his explanation of why he believes this to be v tach. Other well-respected ECG experts have also questioned the original diagnosis. Please refer to the comments below for this very helpful explanation. Unfortunately, this patient is lost to followup, as this incident occurred some time ago.
WTCs remain a most fascinating topic, especially for those who enjoy "detective work". We thank Dr. Grauer, Tom Bouthillet, and others for their contributions to the ECG Guru on this topic.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
LBBB vs V-Tach
Can you describe how this can be differentiated from V-Tach?
Sebastian
LBBB vs V Tach
I agree with Marionurse that atrial activity (p) waves are probably visible in some leads. In addition, the "classic" LBBB pattern is present: wide complexes with a negative deflection in Lead V1 and positive QRSs in Leads I and V6. Sometimes, it can be very difficult to determine the origin of a WCT. In this case, the young patient's history of this illness is a big clue that this is classic SVT. For more on this subject, check out Jason Roediger's discussion on our Ask the Expert page, where he reviews some of the ECG features that make diagnosis easier.
Dawn Altman, Admin
The rhy strip and V3 one can
The rhy strip and V3 one can see aAtrial activity.
Is this Really Supraventricular?
I must admit that I agree with Sebastian and wonder HOW one can be certain that the rhythm strip shown is not VT?
This is indeed an interesting case. I offer the above comments in the interest of academic discussion.
Ken Grauer, MD
Ken Grauer, MD www.kg-ekgpress.com [email protected]
You bring up some very
You bring up some very important points. I do have ECG No 1 somewhere, and will try to find it. The morphology of the QRS complexes supported aberrancy, although of course there is no "proof" in the QRS. Unfortunately, this is a "derived" 12-lead, obtained by a bedside monitor. There are only 5 lead wires, with the precordial leads being placed at the top and bottom of the sternum, and the limb leads on the chest. Even if the electrodes are perfectly placed, there is some alteration in morphology and apparent axis.
The ED physician felt that he was treating an SVT because of the patient's history of being treated with adenosine and released in the past, the past response to Valsalva maneuvers, and the fact that he momentarily broke this rhythm and had a PVC like the one here when the patient tried a Valsalva maneuver. (I did not witness this).
I do recognize that using a derived 12 lead is probably not the ideal situation for a site where experts are analyzing ECGs. They leave much to be desired. I hoped only to demonstrate a WTC that responded to vagal stimulation and adenosine, while remaining stable the entire time. And perhaps a subtle commentary about the fact that the "ideal" treatment - EP study - is not really available to all.
Dawn Altman, Admin
This IS VT after all ... (Did You Catch the Fusion Beat?)
THANKS Dawn for your reply! The GREAT part about ECG Guru is its diversity and receptivity to input and comment from all. The best learning often comes from the difficult cases for which definitive answers are elusive.
That said - I agree with your comment that a derived tracing is far from optimal for assessing QRS morphology where exactitude is extremely important. For readers with an interest - Details at: https://www.kg-ekgpress.com/acls_comments-_issue_11/
One lesson "between the lines" within your reply is one that I've learned the hard way. Regardless of how expert the ED physician referred to in this case may be - IF I am asked to make a clinical decision on which important treatment decisions need to be made - I want to review all relevant data myself. Thus - We really need ECG #1 before we can accept that "previous tracings proved aberrancy".
Taking this one step further - I believe we actually have PROOF that the WCT in this tracing is in fact VT. Look at the very first beat in simultaneously recorded leads V1,V2,V3 (and also rhythm strip lead II at the bottom). This beat is narrower AND smaller in amplitude than EACH of the next 6 beats in the run of WCT. In addition - this 1st narrower beat is INTERMEDIATE in morphology between these next 6 wider beats AND the last beat on the tracing which represents sinus capture. This is because this 1st beat in V1,V2,V3,II is a FUSION BEAT - and that PROVES that the WCT is VT ....
BOTTOM LINE: It IS true that VT is less common in young adults without underlying heart disease. But it is not true that VT never occurs in younger adults. In addition - we do NOT know if this "man in his 30's" had cardiomyopathy or congenital heart disease or something else that may have predisposed him to VT at an early age.
In addition - certain special forms of VT do occur in younger adults. This includes right ventricular outflow VT. While QRS morphology in this case does not resemble that of RVOT (an example of which appears at: http://ecg-interpretation.blogspot.com/2012/01/ecg-interpretation-review... ) - the point is that young adults may have VT. RVOT makes up only a small percentage of all VTs - but it does occur.
There also are Adenosine-responsive VT's (and even some forms of VT that may respond to vagal maneuvers) - so while true that young age and response to adenosine and/or vagal maneuvers clearly makes VT less likely - it does NOT completely rule it out (See - https://www.kg-ekgpress.com/acls_comments-_issue_03/#Adenosine-RESPONSIV... ).
Selection criteria need to be used for determining who to send to EP and who not to send - but in the year 2012 with much greater availability than ever before - to me, the otherwise healthy young adult with more than a single episode of wide tachycardia should be strongly considered for full evaluation. This may be easier said than done given that this patient does not have health insurance - but a phone call to your friendly EP-on-Call for this case while this patient was still in the ED is where I would start.
Finally - I see NO evidence of rate-related BBB from the tracing we are given ...
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Aberrancy with LBBB morphology?
I know this case is little old now, but I'm curious as to how common it is it to see aberrancy resulting in LBBB morphology?
WCT with LBBB aberrancy
I don't know how common LBBB aberrancy is statistically. Various authors state different percentages, or don't try. It is one of the more common forms of aberrant conduction, and is frequently seen in tachycardia, due to the different refractory periods of the left and right bundle branches. This ECG has the appearance of LBBB aberrancy, and, because I was present when the patient was being treated, I believed for years that it was. When you read Dr. Grauer's comments above, however, he presents compelling evidence of this being v tach.
It is important to remember that it is not always possible to differentiate between ventricular rhythms and aberrant conduction. Wide complexes should always be assumed to be ventricular unless there is convincing evidence of aberrant conduction.
Dawn Altman, Admin