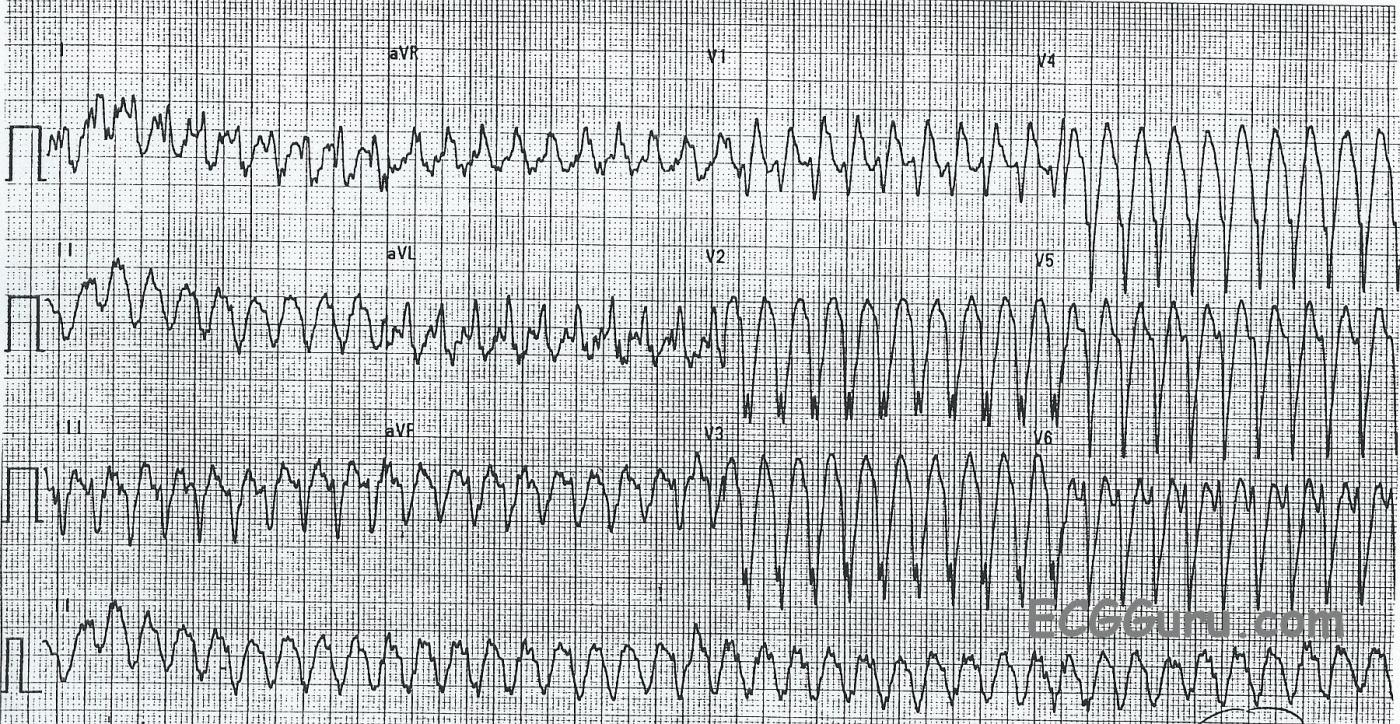
This ECG is from a man who was experiencing palpitations and light-headedness with near-syncope. On first look, you will see a wide-complex tachycardia (WTC) with a rate around 240 per minute. It is difficult to assess for the presence of P waves because of the rate and the baseline artifact.
The differential diagnosis of WCT includes ventricular tachycardia and supraventricular tachycardia with aberrant conduction, or interventricular conduction delay (IVCD). We should ALWAYS consider VENTRICULAR TACHYCARDIA first. If the patient is an older adult with structural heart disease, WCT almost always proves to be VT.
ABERRANT SVT? In the setting of SVT with wide QRS, the most common aberrancy is right or left bundle branch block. This ECG could be said to have a “RBBB” type pattern in V1, rSR’ and in Lead I and V6 with a wide S wave. However, the other precordial leads do not have a RBBB pattern.
VENTRICULAR TACHYCARDIA? There are some features of this ECG that favor the diagnosis of VENTRICULAR TACHYCARDIA (VT). They include, but are not limited to:
* Regular, wide QRS complexes, about .14 seconds in this ECG, but varies because of difficulty in measuring the beginning and end of the QRS in each lead. The artifact obscures the exact points of beginning and ending. The QRS complexes, especially from V2 leftward, are very “ugly”, and don’t resemble patterns we would expect with bundle branch block.
* Horizontal plane axis extremely abnormal: Leads II, III, and aVF are negative and aVR and aVL are positive. The biphasic Lead I indicates a nearly vertical axis at around – 90 degrees.
* There is “almost” precordial concordance, but V1 is biphasic.
Unfortunately, we do not see capture beats or fusion beats, which would secure the diagnosis of VT. Disassociated P waves would also be a sure sign of VT, but the artifact in this ECG makes it impossible to say whether there are P waves.
IDIOPATHIC POSTERIOR FASCICULAR TACHYCARDIA? This tracing also has features of Posterior Fascicular Tachycardia, a type of ventricular tachycardia sometimes called Belhassen-type Tachycardia. These include:
* Borderline QRS width. Fascicular tachycardia usually has a QRS duration of .10 - .14 seconds. (100-140 ms), narrower than other types of VT.
* Short RS interval in the precordial leads. The time from onset of the r wave to the nadir of the S wave appears to be between .04 sec. and .06 sec. The RS interval is usually .10 sec. (100 ms) or more in other types of VT.
* A RBBB pattern, with additional left anterior fascicular block (LAFB or LAHB) pattern. While not typical for RBBB in all the precordial leads, V1, V6 and Lead I suggest a RBBB pattern.
* Left axis deviation, indicating that, if this is fascicular tachycardia, it is arising from the posterior fascicle.
Fascicular tachycardia is an idiopathic tachycardia usually occurring in young, healthy patients, most often male. There is a lack of structural heart disease, and the tachycardia usually occurs at rest. The mechanism is re-entry of an ectopic beat from the left ventricle. It often responds to the use of Verapamil, rather than the usual drugs used for SVT and VT.
BOTTOM LINE When faced with a patient with wide-complex tachycardia, the more information you have, the better. That includes patient history, family history, medications, signs and symptoms. A 12-lead ECG may prove to be invaluable, unless the patient is so severely unstable that there is no time. It can be very difficult to diagnose a WCT from these tools, and electrophysiology studies may prove beneficial.
ALWAYS TREAT WCT AS VENTRICULAR TACHYCARDIA UNTIL IT IS PROVEN TO BE SOMETHING ELSE.
Of course, we would welcome a discussion on this topic, sign in to comment below. (Sign in is necessary for our efforts to repel SPAMMERS.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
A Regular WCT Rhythm with Atypical QRS Morphology
One of the most important diagnostic dilemmas in ECG interpretation entails assessment of a regular WCT ( = Wide-Complex Tachycardia) rhythm. The tracing presented here provides an excellent example of this.
I agree with the points made in Dawn’s discussion. I’ll simply add a few additional comments that serve to amplify the approach I previously suggested in the 3/19/2015 ECG Guru Instructor Collection Tracing:
Although we do not know the age of the patient in this case, nor whether this patient has a history of underlying heart disease — we DO know that this man was clearly symptomatic (palpitations with light-headedness and near-syncope). Thus, regardless of whether the rhythm is ventricular or supraventricular in etiology — immediate cardioversion is indicated — and, after conversion to sinus rhythm — full evaluation with consideration of EP (ElectroPhysiology) referral is in order.
The literature suggests that the statistical likelihood that a regular WCT rhythm without sign of sinus P waves is VT is at least 80%. Several features in this case increase those odds. As Dawn mentioned, QRS morphology in leads V1, I and V6 is consistent with a RBBB pattern. However, the entirely negative QS complex in leads V2-thru-V5 is unlike any normal RBBB pattern. In addition — the QRS complex in lead II is all negative — and, the QRS is all positive in lead aVR. Therefore, QRS morphology is highly suggestive that this rhythm is VT.
It is of interest that a number of leads on this tracing suggest the presence of atrial activity. This is perhaps best seen in the long lead II rhytm strip at the bottom of the tracing. That said, if the extra notching seen near the beginning of the T wave does reflect atrial activity — this does not help in distinction between VT vs SVT (SupraVentricular Tachycardia). That’s because there is no AV dissociation. Instead, the RP’ interval (ie, distance from the QRS until the notch in the T wave that follows) remains the same. Both VT and reentry SVT rhythms may transmit back to the atria with 1:1 VA (ie, retrograde) conduction.
Finally — the very fast ventricular rate of ~240/minute is worthy of comment. Both VT and SVT rhythms may conduct this fast, as can AVRT (Atrio-Ventricular Reentry Tachycardia) in which the reentry SVT rhythm travels anterograde (ie, down in the forward direction utilizing an accessory pathway). Of interest, EP cardiologists have noted that as an SVT rhythm attains these very fast ventricular rates — aberrant conduction sometimes fails to resemble the QRS morphology of a typical conduction defect. That’s because of much greater dispersion of refractory periods within the conduction fascicles at these very fast rates. That said — QRS morphology in this example is so atypical, that my strong hunch remains that this rhythm is Venricular Tachycardia until proven otherwise in the EP lab. But, because of this very-rapid-rate phenomenon and, resemblance in leads I, V1, V6 of a RBBB-pattern — IF this patient was hemodynamically stable, my initial intervention would probably be a trial of IV Adenosine prior to cardiovesion. Unfortunately, no follow-up on this case is available.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
WCT: "Woefully Confusing Tachycardia"
Dawn...
Thanks for another challenging wide complex tachycardia.
At first glance, we always tend to lean toward VT as the cause of a wide complex tachycardia. And with good reason: 1) if we knew nothing at all about this patient other than he/she had a wide complex tachycardia and we assumed it was VT, we would be correct 80% of the time. 2) If we knew that the patient had a history of heart disease (MI, angina, CHF, cardiomyopathy) and presented with this ECG and we assumed it was VT, we'd be correct 95% of the time! So it is not without some academic support that we tend to "want" to diagnose VT. And there is also a reassuring psychological boost for the person treating the patient: once we resolve that it is VT we can go ahead and treat the patient which usually means a dose of some "Edison medicine" rather than an IV antidysrhythmic medicine. Besides, generally whatever will treat VT will also treat SVT with aberrancy.
However, there are times when the diagnosis just doesn't want to conform to our preconceptions. Take this ECG, for instance...
When I use the Brugada criteria to analyze it, here's what I see...
Therefore, as much as this tracing looks like VT, if we adhere to the Brugada criteria, it is SVT with aberrant conduction.
In their landmark paper on the criteria and algorithm, the Brugadas include an ECG that is almost exactly the same as this one and they come to the same conclusion. Both ECGs appear to have a LAFB and LAFB can result in an R/S ratio < 1.0. They make no mention of fascicular blocks or fascicular tachycardias in their paper.
Also, I would like to point out that NO CRITERIA for distinguishing VT from SVT with aberrancy ever mention AGE. Don't let the fact that a patient is in his or her 20's dissuade you from a diagnosis of VT if the criteria fit.
Dawn, thanks again for a great learning ECG and a wonderful website.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
Woefully Confusing, indeed
Oh, how I wish we had more patient information, especially EP lab results! This is just one of many WCTs in my collection that have been argued by great minds. For the reasons stated by both Drs. Grauer and Jones, I have always felt comfortable in the clinical emergency setting to "treat as VT until proven otherwise". Fortunately, it was never my responsibility to get to the true etiology later. And, early in my career, we didn't even HAVE EP labs!
Thank you both for a very stimulating discussion.
Dawn Altman, Admin
My Comment in Response to Dr. Jones
My thanks to Dr. Jones for making discussion of this tracing even more interesting than it already was! There are indeed many criteria in the literature for assessment of the regular wide-complex tachycardia (WCT). It is true, that if one adheres strictly to the Brugada algorithm that Dr. Jones refers to — that the answers to each of the 4 Steps in the Brugada approach are “No” — so that IF one adheres solely to this algorithm — then one would conclude that this rhythm is SVT.
That said, there are 12 leads on this 12-lead ECG — and 3 of these 12 leads would seem strongly suggestive of VT. The finding of an entirely upright, monophasic R wave in lead aVR is highly specific for VT. The finding of an all negative QRS complex in lead II in the setting of an otherwise indeterminate front plane axis during a regular WCT without P waves is also highly suggestive of VT. Finally, while true that leads V1 and V6 are not helpful in morphologic assessment of this WCT (as per Dr. Jones) — the all negative QRS in leads V2,V3,V4 (and almost all negative QRS in V5) are clearly neither suggestive nor consistent with RBBB aberration by any of the usual standards for making that diagnosis. I therefore would argue that on a morphologic basis — the WCT rhythm shown here is distinctly atypical for any form of conduction block, and therefore unlikely on morphologic grounds to be an aberrantly conducted SVT.
That said, EP cardiologists have observed in the laboratory that highly unusual QRS morphologies may be observed with aberrant conduction when the ventricular rate is extremely fast. The rate of 240/minute as seen here would seem to qualify for this phenomenon. BOTTOM LINE — Whether due to some morphologically atypical form of aberrant conduction or anterograde AVRT or VT — the clinically important points I hope Dr. Jones agrees with me on regarding this tracing are: i) that we cannot be 100% certain of the ECG diagnosis in this case; ii) that if the patient is hemodynamically unstable at the time of this tracing — that immediate electricity is indicated; iii) that if the patient was hemodynamically stable — that empiric treatment with Adenosine would be a reasonable initial option; and iv) that definitive diagnosis of the etiology of this arrhythmia might not be obtained until some later point after the patient has been converted out of this rhythm.
THANKS to Dr. Jones for his stimulating discussion. We invite additional comments from others!
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Thank You, Dr. Grauer!
I'm always flattered when someone reads one of my posts and thinks enough of it to comment. In actuality, Dr. Grauer, I really don't think we disagree much, if at all. If one follows the Brugada criteria, as stated by the Brugadas, this is the result you get. I am well aware of the Sasaki and Vereckei algorithms as well as all the older ones. If I am not mistaken, I don't think any criteria or algorithm has a consistent 100% specificity following validation studies (the Brugada certainly doesn't). I have seen so many WCTs with such problematic morphologies that were basically unexplainable (at least by me) that I don't think we can let such inconsistencies stymie us in our search for plausible interpretations. When there is a disagreement between algorithms, we have to remember that the person providing treatment is still the ultimate authority and that a decision must be made, whether based on statistics, published algorithms, experience or even (gasp!) a physical exam. We can never be 100% accurate because none of our "tools" are 100% accurate. In response to your numbered comments:
1. I think it would be very rare to be able to say with 100% certainty that any rhythm is VT or not and that certainly applies to this ECG. I think only an EP lab would be able to figure that out.
2. If the patient is hemodynamically unstable, the last thing a physician, nurse or paramedic should be doing is trying to interpret an ECG. Time is not just myocardium, it's also brain and kidneys! Electrical cardioversion is the ultimate treatment as well as being the fastest and most successful. And, when done properly, it is the safest. But absolutely, if the patient is hemodynamically unstable, your course is already determined.
3. In any patient with a rapid, REGULAR WCT adenosine is certainly a very reasonable option. As much as they hate adenosine, I think every patient would opt for the adenosine instead of the paddles!
4. Later diagnosis is certainly a possibility, but I wouldn't be too hopeful unless the baseline ECG reveals a BBB or some other inter- or intraventricular conduction problem.
Thank you again, Dr. Grauer, for your insight and input. I have been a big fan of yours for some time.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
Glad we Agree!
Thanks Dr. Jones! I do think we agree — and glad we could use our perspectives to amplify the discussion.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Jones's Perplexium
After reading over all the comments (including my own) several times and reading quite a few similar discussions on other blogs and websites, I noticed something:
In the medical field - though this could apply as well to science in general or even business and political decisions - we tend to make decisions and THEN seek support for what we have already decided. I am referring to experienced physicians, nurses, PA-Cs and paramedics who carefully and thoughtfully look at an ECG, for instance, like the one with the wide-complex tachycardia posted on this site and, realizing that an immediate and confident diagnosis is not going to be obvious, then turn to one of a number of criteria and/or algorithms to try to distinguish a true ventricular tachycardia from the other diagnostic possibilities.
In fact, let's look at this ECG specifically. We are going to assume that the patient is very stable hemodynamically and well-oriented since otherwise there is only one decision to make: "How many joules?" There are a number of criteria and algorithms that can be used. All have some merit but none are 100% reliable. That is usually the situation no matter what the medical, scientific or business problem may be.
Let's say your impression is that the patient has a ventricular tachycardia. You then use Criteria/Algorithm A to see if it distinguishes between VT or "other dysrhythmia." Let's say it tells you that it is not VT. What do you do now? Do you accept that diagnosis or do you use Criteria/Algorithm B? Let's say that Criteria/Algorithm B diagnoses VT. What do you do now?
Even if Criteria/Algorithm B has a higher probability of being correct (let's say it is correct 75% of the time) and Criteria/Algorithm A has a 65% probability, neither really answers the question "Is this VT?" Each also has a probability of being wrong and while the one with a greater probability of being correct is the better choice if one HAS to choose, once having chosen one should still be less than 100% confident of having achieved the correct diagnosis - even though the proper decision was made given the circumstances.
My point is that whether we feel we know the diagnosis or not, before using any criteria or algorithm we have already decided what our diagnosis is going to be. If the first algorithm doesn't produce the result we expect, we tend to move on to another algorithm until we find one that DOES support our diagnosis and at that point we are suddenly "justified" in recording our diagnosis and acting upon it. Had one simply acted on one's first impression, the likelihood that the same treatment plan would have been arrived at much earlier is extremely high (I certainly have done no studies on this but I would surmise it to be very high!). Most people who feel that a patient has a VT are not going to accept an algorithmic diagnosis of SVT - they will keep looking for a justification for diagnosing VT when they've had the diagnosis and the justification all along. I maintain that anyone whose first impression of a rhythm is VT is NOT likely to accept an algorithmic decision of SVT. It's probably best to go ahead and treat - which may include a trial of adenosine before cardioversion (remember: our patient is very stable hemodynamically).
I suppose "Jones's Perplexium" is that we tend to make our decisions first and then seek support for them by running more tests or utilizing more algorithms. Our thought processes should be characterized by an inverted triangle with a large amount of information eventually being reduced down to a diagnosis or decision when instead, it is too often just the opposite: a diagnosis or decision followed by a lot of data (often selected with a bias) in order to justify the diagnosis. The simplest way to understand this is to ask yourself: "If I looked at a wide complex tachycardia and felt that it could be VT, would I stop at using just one algorithm if the algorithm diagnosed 'non-VT' or would I continue with another algorithm?" If you are going to keep looking until you get the answer you "want," then why waste time looking at all?
The wide complex tachycardia here satisfied two different criteria with two very different outcomes. The bottom line is that although no one interpreting this ECG felt totally confident of a diagnosis, in the real world a decision would still have to be made and treatment rendered. And while a definitive answer may only come via a trip to the EP lab, that isn't going to happen in real life.
Jones's Perplexium does not apply when one IS completely confident of the diagnosis and consequently has no need for algorithms or extensive testing.
I would like very much to hear other's thoughts on the process of decision-making. I'm not talking about the merits of specific WCT algorithms, but the way we approach our decision-making.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
Agree Dr Jones
i agree with you, and plead guilty. As I read your last comment, I was formulating my own comment, and it was almost word-for-word your paragraph near the end about the "bottom line". Like you, I spent many years in the ED (as a nurse). Decisions often had to be made quickly - not just in unstable situations, but because there were so many patients and so few of us. We wanted to start care safely, then turn it over to the next caregivers.
When I looked at this ECG, my first feeling was "VT" because of the axis and a lack of "typical" RBBB after V1. I went through all the criteria I was familiar with, and some I wasn't. Some indicated that this was most likely SVT, some VT. Yet I included "VT" in the title of the post. Realistically, I realize that only in the EP lab will this mystery be unraveled. But, I feel confident in the treatment algorithm for stable and non-stable patients.
You certainly have me questioning my decision-making process I plan to be more aware of this in the future Thank you to both you and Dr Grauer for a very interesting conversation
Dawn Altman, Admin