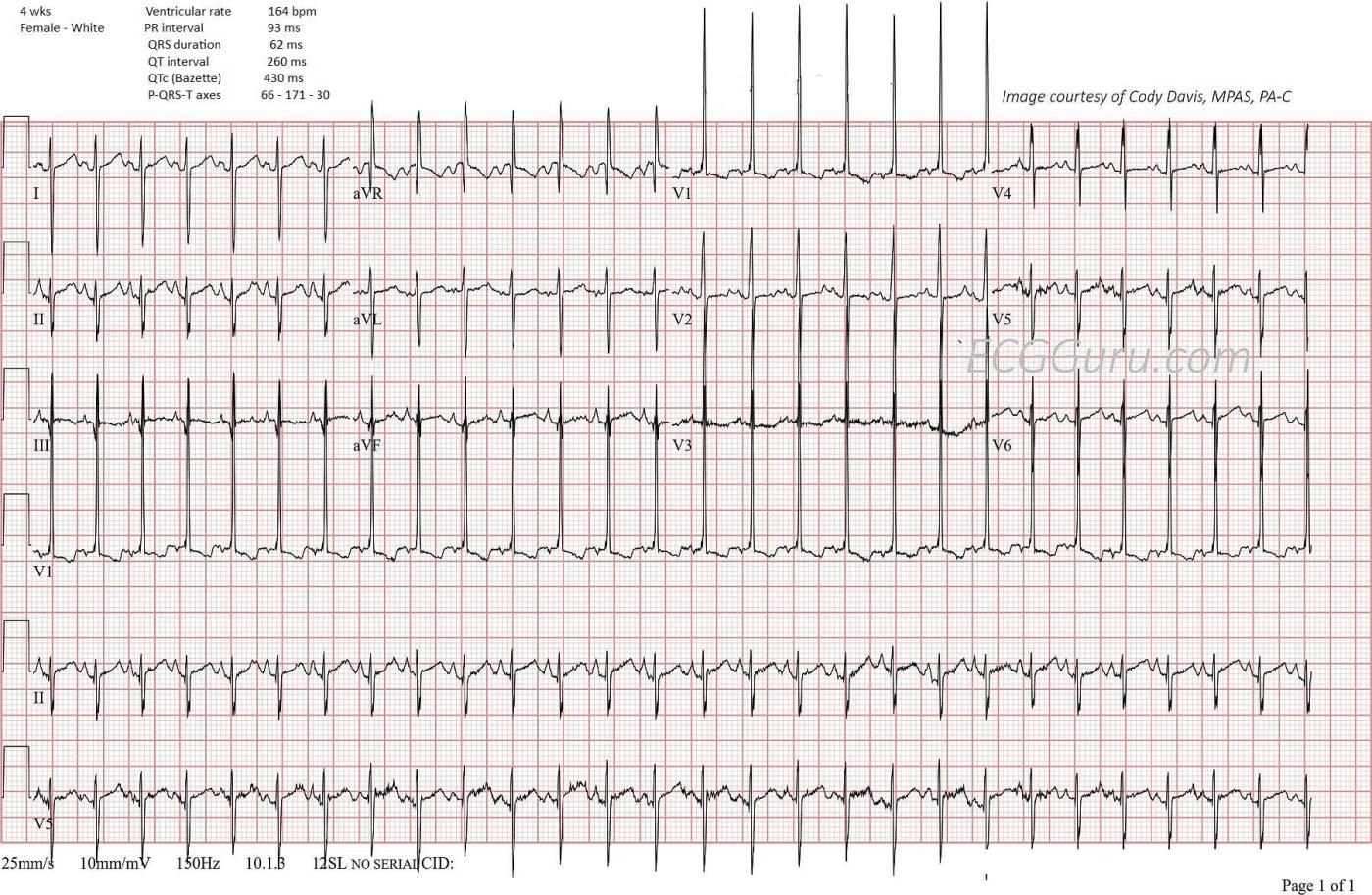
The patient: 4 week old female infant with past medical history of meconium aspiration at birth with APGAR scores of 2,4,6. Intubated and given nitric oxide for pulmonary hypertension. Weaned in NICU over 10 days. Echocardiogram during that time showed stiff pulmonic valve. This ECG was obtained at follow up appointment. Infant is eating well, no cyanotic spells. Four- week echo continues to show pulmonic valve stenosis. We do not know chamber measurements. Patient scheduled for a balloon valvuloplasty.
Babies are born with relatively symmetrical hearts. Unlike adult hearts, the right ventricle comparatively large due to the work it has to do to pump against the high pulmonary pressure before birth. Because newborns’ hearts are more to the right side, we often do right-sided chest leads in addition to the standard 12-lead ECG.
The ECG: In spite of the pulmonary valve stenosis, this ECG is within normal limits for this 4-week old. Some of the ECG findings here that would be abnormal for an adult ECG, but are normal for this 4-week-old baby are:
· The rate is on the high side of normal, but we do not know her level of activity or excitement (is she crying?).
· Her lead II P waves are upright, and possibly tall enough to consider P pulmonale (> 2.5 mm).
· The QRS complexes are very narrow and the PR interval is short, both of which are normal for this age.
· The corrected QT interval is within normal limits.
· There are septal Q waves in Leads II, III, aVF, V5 and V6 (hard to be sure because of artifact.) This is normal for infants, and these are not “pathological Q waves”.
· The QRS axis is rightward at 170 degrees, which is on the high side of normal range for a 4-week-old. This reflects the relatively large size of the right ventricle.
· There are prominent R waves in the right precordial leads, again reflecting the relative size of the RV., possibly to the point of being abnormally enlarged.
· The T waves in V1 are inverted, and biphasic or flat in V2 and V3 (again hampered by artifact).
The echocardiogram is a much more accurate measure of RV size and strain than the ECG.
I am not a pediatric ECG expert by any stretch of the imagination. I would welcome any readers who are to add to this summary and let me know what I have missed. I am also including some links to resources on the topic.
Many thanks to Cody Davis, MPAS, PA-C, for donating this ECG to the ECG Guru.
1. Saidi, Arwa, MB. FAAP. FACC. Electrocardiograms and Top Ten Neonatal Arrhythmias. (2015) https://neonatology.pediatrics.med.ufl.edu/files/2016/05/Neonatal-ECG-Talk.pdf Accessed September 27, 2023.
2. Ge Health Care. How to Approach and Interpret Pediatric ECG, (2022) https://www.gehealthcare.com/insights/article/how-to-approach-and-interpret-pediatric-ecg Accessed September 27, 2023.
3. Tipple M. Interpretation of electrocardiograms in infants and children. Images Paediatr Cardiol. 1999 Jan;1(1):3-13. PMID: 22368537; PMCID: PMC3232475. https://ncbi.nlm.nih.gov/pmc/articles/PMC3232475/ Accessed September 27, 2023.
4. ECG & Echo Learning. Pediatric and Neonatal ECG Interpretation https://ecgwaves.com/topic/practical-pediatric-ecg-interpretation/ Accessed September 27, 2023.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Pediatric RVH on ECG — A Special "Specialty"
I was asked for input on today's ECG by Dawn — of a 4 week old female infant with known pulmonary hypertension.
The ECG interpretation of pediatric tracings is an art unto itself. I fully acknowledge no special expertise in this area. That said — I have researched this topic, and have written some basic overviews for adult providers wanting some background in "The Basics" of Pediatric ECG interpretation. I provide the following links for those with an interest — while fully advising consultation with pediatric cardiology when clinical questions arise.
My Chapter, "When the Patient is a Child" (from Grauer K: Practical Guide to ECG Interpretation [2nd Edition] by Mosby, St. Louis, 1998, pp 272-283 (https://tinyurl.com/KG-Peds-ECG ).
2 Reference Tables from Rijnbeek et al: Eur Heart J 22(8): 702-711, 2001
Pediatric R Wave Upper Limits by Age — https://tinyurl.com/Peds-ECG-R-Wave
Pediatric S Wave Upper Limits by Age — https://tinyurl.com/Peds-ECG-S-Wave
Regarding today's tracing — I'll begin with the caviat that the tiny chest of young infants makes reproducibly accurate voltage measurements highly challenging! Echo is clearly superior for assessment of cardiac chamber size, and especially for structural abnormalities. That said — the ECG may provide useful information in the pediatric age group for chamber size based on norms for age regarding axis and QRS amplitudes.
I interpreted today's ECG as highly suggestive of significant RVH. There is marked RAD (Right Axis Deviation) of at least +150 degrees — ECG critieria for RAE (tall, peaked and pointed P waves ≥2.5 mm — which is easily assessed by noting that P wave amplitude in lead II is at the very least half of a large box tall) — and a huge predominant R wave in lead V1 that I measure to be ~28 mm. Assessment of S wave depth in lateral chest lead V6 is difficult because of the overlap with the long lead V1 rhythm strip below it — but these lateral chest lead S waves are also deeper than typically expected.
This child with pulmonary stenosis clearly needs the expertise of a pediatric cardiologist. I thought her ECG suggests significant RVH consistent with her diagnosis.
Ken Grauer, MD www.kg-ekgpress.com [email protected]