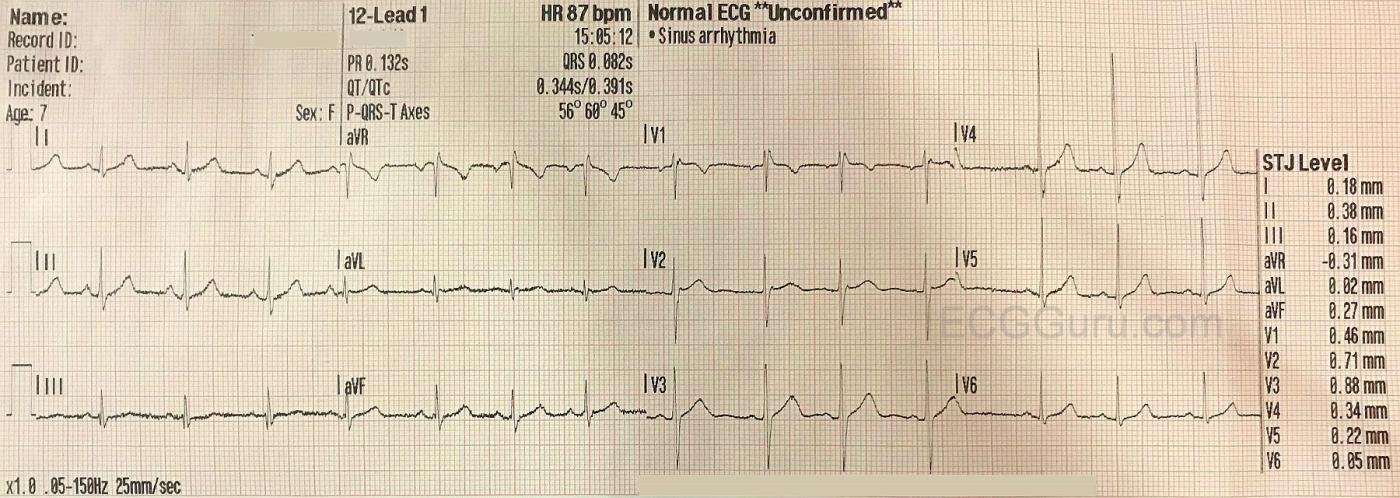
The Patient: This ECG was obtained from a seven-year-old girl who was complaining of mild, non-specific chest pain. A medical workup found no structural or electrical abnormalities, and her pain resolved without treatment. This is a good ECG to illustrate some of the ECG findings that are normal at this age, which might not be normal in adults or in infants.
The ECG: A general description of this ECG would include:
· Normal sinus rhythm at 87 bpm
· Normal frontal plane QRS axis at 60 degrees
· PR interval: .132 second (132 ms)
· QRS duration: .082 second (82 ms)
· QTc: .391 second (391 ms)
· Predominantly negative V1 and positive V2
· Slightly irregular rhythm with no apparent changes in P wave morphology
· Very subtle J point elevation in V1 through V3
The Normal ECG in Children It is not really possible to state exact parameters for pediatric ECGs by age alone. ECG findings are affected by age, but also by race, gender, body size, and puberty. There are some findings in this ECG that can be considered to be normal for this child without being necessarily normal for an infant, or for an adult.
· The slightly irregular sinus rhythm is very common in children
· T wave inversion in V1 is normal for a 7-year-old. In infants older than one week, T waves are usually inverted in V1 – V3. The right precordial T waves will become upright during early childhood, with V3 becoming upright before V2.
· RSR’ pattern in V1 resembles right bundle branch block without the QRS widening.
· Tall R waves in mid-precordial leads may appear to meet voltage criteria for LVH. However, there is no “strain” pattern in the ST segments. In this example, there is also no left axis deviation and aVL has low voltage (normal). This appearance of high voltage is due to the child’s small chest wall, which makes the heart’s voltage readily measurable by the surface leads. (The ECG, in general, is not the best way to diagnose LVH – imaging is much better).
· Slightly peaked (rather than rounded) P waves, less than 3 mm in height.
Some findings that might be normal in a seven-year-old that are NOT present in this ECG include:
· Ventricular or supraventricular ectopy
· Slightly rightward frontal plane axis
· Dominant R wave in V1 (although the R wave in V2 might be taller than expected in an adult).
· Short PR interval and QRS duration.
· PR interval variations.
References: For more information, go to:
Heart. 2005 Dec; 91(12):1626-1630. Doi: [10.1136/hrt.2004.057307]
PMCID: PMC1769212
Life In The Fast Lane Paediatric ECG Interpretation
Many thanks to Alan Vinyets for donating this ECG to the ECG Guru.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Some Thoughts on Interpreting Pediatric ECGs
Many emergency providers do not see pediatric ECGs on a regular basis. As a result, they are less familiar with what to expect on those occasions when the ECG in front of them is obtained from a child. Even as the Attending tasked with reading all ECGs obtained in a 35-physician primary care clinic over a 30-year period — the number of pediatric ECGs I was asked to interpret was limited (usually to no more than 1-2/month).
— As a guide to the Basics of Pediatric ECG and Rhythm Interpretation — I developed these 2 user-friendly pdfs. For those with limited experience in this area — these brief pdfs may help get you started.
— As to the ECG in this case — I interpreted this tracing as “Normal for Age”.
— The rhythm is sinus arrhythmia. This rhythm is “the rule” rather than the exception in a pediatric age group.
— All intervals (PR, QRS, QT) are normal. As discussed in the above pdfs — the limits for intervals vary depending on the age of the child. They are normal here.
— The frontal plane axis is normal.
— There is no chamber enlargement.
— There is an rSr’ pattern in lead V1. This is also an extremely common finding in children, as well as in young adults. It’s possible there may be some degree of lead misplacement — since the finding of a significant negative component to the P wave in leads V1 and/or V2 + an rSr’ in these leads, with a PQRST appearance in lead V1 that looks very much like the PQRST appearance in lead aVR is often seen when leads V1 and/or V2 are placed 1 or 2 interspaces too high on the chest. Achieving accurate lead misplacement is of course a challenging endeavor given the small chest dimensions of many young children — but it’s good to be aware that lead malposition of lead V1 is a possibility here.
— Otherwise — the fact that in addition to the rSr’ pattern in lead V1, there are terminal s waves in both leads I and V6 may indicate IRBBB (Incomplete Right Bundle Branch Block). That said, IRBBB is common in young patients. Rather than representing a conduction defect — IRBBB often merely reflects slight delay in depolarization of the right ventricular outflow track which is not necessarily abnormal.
— There is early transition (ie, the R wave = S wave amplitude early, between lead V1-to-V2). In the context of an otherwise normal tracing, this is merely a descriptive finding.
— Finally, NOTE — there is an rsR’s’ pattern in lead III. This multideflection pattern is unlikely to be abnormal given the otherwise unremarkable findings on this tracing.
BOTTOM LINE: This ECG is “Normal for Age”.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Two More Thoughts on Pediatric ECGs
An excellent reminder that adults aren't the only ones who get ECGs. All the comments are very informative. Like Dr. Grauer, although I have been reading ECGs for many years, relatively few were pediatric ECGs. The only extra advice I can give refers to two things:
1) Beware of "narrow complex" tachycardias in young children. All children aged 8 yrs and younger should have QRS intervals that are no greater than 0.08 sec (80 msec, just remember "80 under 8"). If the QRS is wider than that in that age group you are probably dealing with a wide-complex tachycardia.
2) Be aware of the most common possible findings in the pediatric ECG and don't be surprised when you see them. However, on the other hand, don't be surprised if you DON'T see them. In my own, personal experience, the vast majority of ECGs that I saw in young children (around age 2 yrs and up) looked more like adult ECGs than classic pediatric ECGs.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd