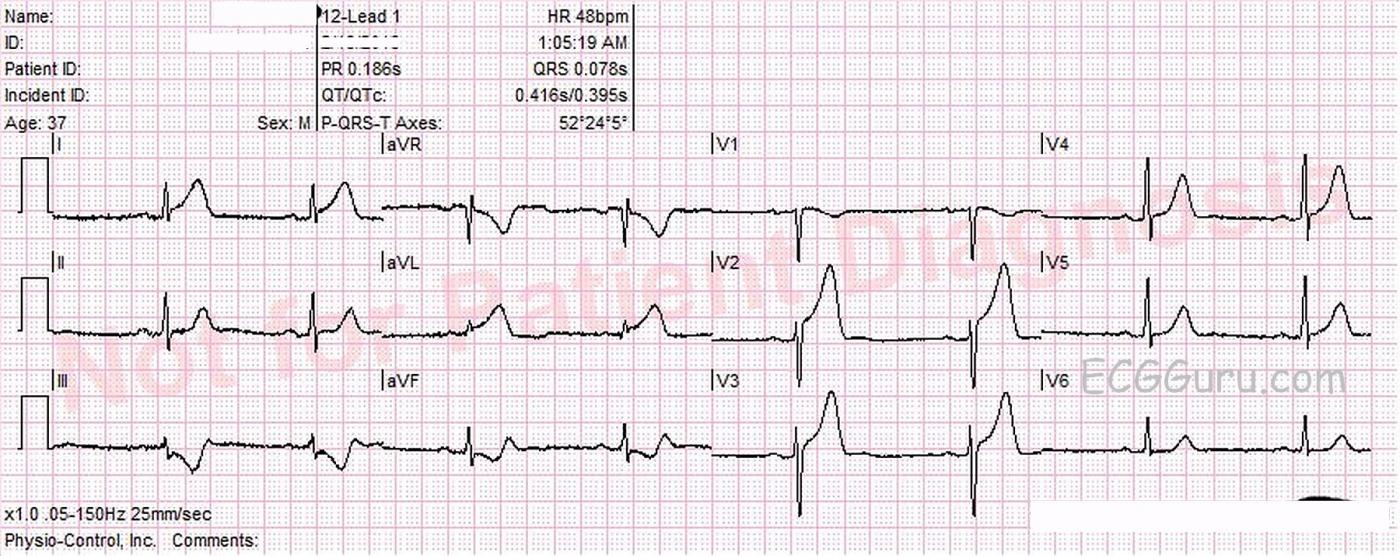
This ECG was obtained from a 37-year-old male who was complaining of non-radiating substernal chest pain. He offered no significant medical history. He denied taking any medications. He was hypertensive and bradycardic on arrival in the Emergency Dept. He was alert and ambulatory. Approximately 20 minutes after first being seen by paramedics, he suffered an episode of ventricular fibrillation in the E.D. He was resuscitated and sent to the cath lab. His coronary arteries were without lesions. We do not know the results of any lab tests, including troponins.
What does the ECG show? The rhythm is sinus bradycardia at a rate of 48 bpm. The PR, QTc, intervals and QRS duration are normal. The QRS frontal plane axis is normal and there is good R wave progression in the precordial leads. There is ST segment elevation in Leads I, aVL, V2, and V3, with reciprocal ST depression in Leads III and aVF. The ST segments that are elevated retain a relatively “normal” shape, being concave upward. There are no abnormal T wave inversions or pathological Q waves.
Discussion While this ECG is certainly consistent with the diagnosis of anterior-lateral M.I. (STEMI), the patient was found to have “clean” coronary arteries. Any adult presenting with chest pain and ECG abnormalities should be assessed for acute M.I., of course, and that often involves a trip to the cath lab. Most acute M.I.s are caused by a ruptured plaque in a coronary artery that has formed a blood clot and obstructed blood flow through that artery. Other conditions can cause blood flow obstruction, such as coronary artery spasm. An imbalance in supply and demand can also damage the heart muscle, even if not caused by thrombus. A general term for an M.I. (confirmed by troponins, echocardiography, or catheterization) is “MINOCA”, “myocardial infarction with non-obstructive coronary arteries”. It can occur in up to 10% of patients presenting with clinical features that are diagnostic of STEMI. There are many examples of MINOCA, including, but not limited to, spasm, cardiomyopathies, or thrombotic disorders. Because of this patient’s presenting symptoms and subsequent episode of V Fib, we are confident that he received a thorough investigation of possible etiologies, but unfortunately, we have no results.
Please comment below to add to this discussion. We are very interested in your experiences with MINOCA.
Many thanks to Lew Steinberg and the Palm Beach Gardens, FL Fire Rescue Department for donating this ECG.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Looks like a STEMI — but a lack of follow-up …
As per Dawn — this ECG shows sinus bradycardia and arrhythmia with hyperacute ST-T waves + significant ST elevation in anterolateral leads + “mirror-image” reciprocal ST depression. In a patient with new-onset chest pain — this ECG picture strongly suggests acute proximal LAD occlusion (from acute evolving anterolateral STEMI). Unfortunately, lack of follow-up, other than report that “the coronary arteries were clean” leaves us hanging with many more questions than answers … Was cardiac cath truly normal? Was troponin increased? What did subsequent ECGs show? In addition to coronary spasm — a myocardial bridge could produce this picture of transient coronary occlusion that subsequently resolves and goes undetected (potentially without underlying coronary disease in a previously healthy 37 yo). Beyond this speculation — I have little more to add. A shame not to have more follow-up on what otherwise is a great case …
----------------
P.S. (4/17/2018): For more on "myocardial bridging" — Please check out my ECG Blog #150 — :)
Ken Grauer, MD www.kg-ekgpress.com [email protected]
My own experience as an emergency physician...
I recall a few scenarios like this during my years as a practicing emergency physician (except I don't recall any of them having a cardiac arrest while in the emergency department). Like this patient, they were all admitted to cardiology and all we could find out was that the cath was negative.
What I (unfortunately) observed over the years was that once cardiology determined there was no MI or at least no lesion to treat, the patient was given a clean bill of health. However, this "clean bill of health" was only from the cardiologist's perspective and the patient too often assumed that nothing was wrong. Lack of a finding by the cardiologist does NOT mean nothing is wrong. I personally know of four cases where the patients sought no further medical care until their GI cancer was too far along to treat effectively.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
Wow. Excellent point.
Thanks, Dr Jones. A good reminder that patients WANT to hear good news (of course) and will often run with that. Symptoms warranting an ED visit should be thoroughly evaluated.
Dawn Altman, Admin
Test comment
Hello! This is a test comment
Webmaster of ECG Guru | View Website