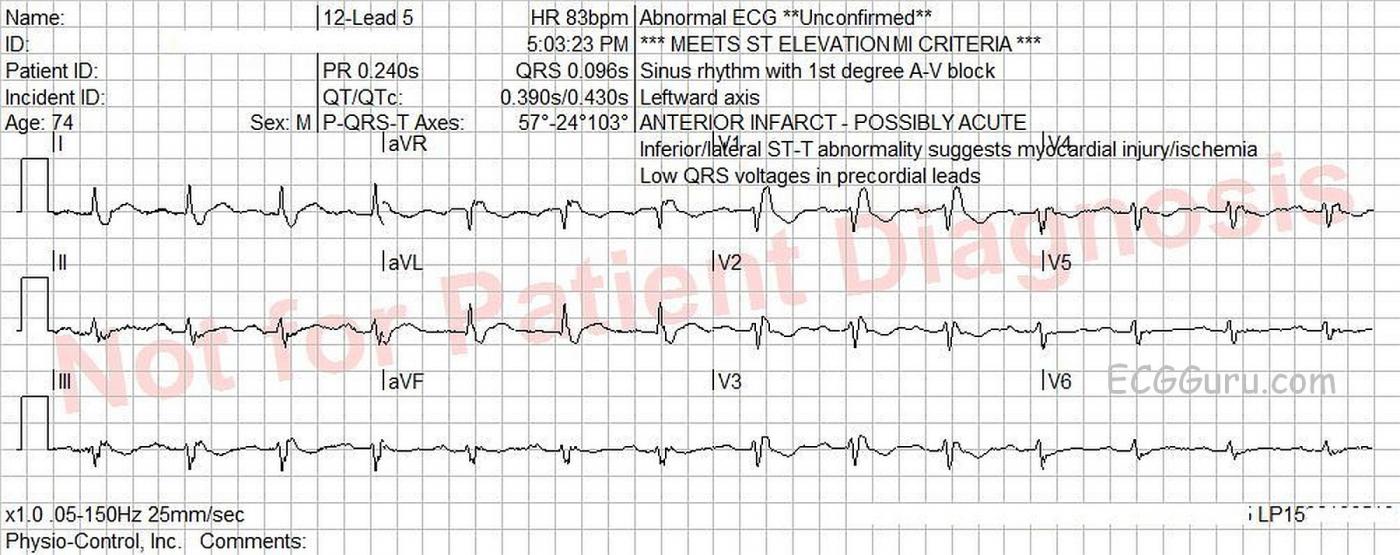
Today’s ECG is from a 74-year-old man for whom we have no clinical information. It shows a “classic” right bundle branch block. It also shows an example of the ECG machine getting some of the interpretation wrong. An early mistake in the interpretative algorithm caused a cascade of inaccuracies.
REVIEW of RIGHT BUNDLE BRANCH BLOCK ECG CRITERIA
* Supraventricular rhythm
* QRS .12 seconds (120 ms) in width
* rSR’ pattern in V1
* Small, wide S wave in Leads I and V6
In right bundle branch block, the initial part of each QRS complex represents the depolarization of the septum and left ventricle. The right ventricle depolarizes late, and is represented by a terminal wave at the end of each QRS. In V1, that terminal wave is the R’ and in I and V6 it is the small S wave.
MACHINE MISTAKES The first mistake the machine made was in measuring the QRS width. The machine says the QRS is .096 seconds (96 ms). It is actually about .16 - .18 seconds. Look at the second QRS in V1, and you will see that it extends almost the full width of a wide block (.20 sec). It is apparent that the machine measured only the left ventricular portion of the QRS complex. Because of this error, the right bundle branch block was not noted.
The mistake in measuring the QRS complex resulted in the machine misinterpreting the terminal wave as the ST segment. This resulted in notations in capital letters warning of ST elevation and presence of myocardial ischemia. The j points are actually at the baseline in all leads, indicating NO ST elevation.
ST and T WAVE CHARACTERISTICS OF RBBB Typically, in RBBB, the T wave will be opposite in direction from the terminal (RV) deflection. So, when there is an R’, there will be T wave inversion. The j point of the ST segment will not be altered, as the ST segment reflects what is happening in the LEFT VENTRICLE, which is depolarizing normally. That means that an acute ST elevation M.I. will look the same in RBBB as it does without BBB.
OTHER FINDINGS With the artifact, and the lack of “small blocks” marked on the ECG paper, it is difficult to say for certain what the P wave width and voltage is, but it is suggestive of P mitrale, or left atrial enlargement. There is a first-degree AV block, with a PR interval of .24 seconds. The axis is slightly leftward, but criteria for left anterior fascicular block are not met. And there is low voltage in precordial leads, and inferior leads. Clinical correlation, including the body size of the patient, would be needed to determine the significance of these abnormalities.
The ECG machine’s interpretation can be very helpful. At times, it will remind us to look for something we have forgotten to consider. However, it should never be used exclusively for ECG interpretation. There are many mistakes made by interpretative algorithms, and there is no clinical correlation used except for age and gender.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
RBBB, LAA, Computerized ECGs — and MORE!
This case brings up a number of important points:
i) Bad data in = Bad data out ... Resolution of this tracing is extremely poor. As a result, it is not unexpected that computerized assessment of poor data may also be poor. In an "ideal world" — somewhat better resolution should be sought when purchasing ECG machines.
ii) Computerized ECG interpretation CAN be useful — IF they are used correctly. But clinicians need to be aware of what the computer can and cannot do well. I present my approach to optimizing use of computerized ECG interpretation in my ECG Blog #126.
iii) The ECG is neither sensitive nor specific for the diagnosis of atrial enlargement (especially for diagnosis of left atrial enlargement). As a result, I favor underdiagnosis of atrial abnormality. My degree of certainty about P wave widening on this poor resolution tracing is not high. As a result, I probably would not indicate “LAA” — though I realize others may differ. My approach to assessing for atrial abnormality is reviewed in detail in my ECG Blog #75.
iv) Complete RBBB is present on this tracing for the reasons Dawn mentions. That said, we LACK a history in this 74-year old man. While a history is always essential for optimal clinical interpretation of any ECG — it is especially important in this case. That’s because there are some subtle findings that could potentially be significant! In both lead I and lead aVL — the J-point (that occurs just after the wide S wave in these leads) looks like it might be slightly elevated. In lead II, the J-point and beginning of the ST segment look like they may be slightly depressed (which therefore could potentially reflect a “reciprocal” change). And in leads V5 and V6 — the ST-T wave is clearly flat, whereas we should normally see a definite upright T wave. Finally, there is still some T wave inversion in lead V4 — whereas normally with RBBB, ST-T depression does not persist this far over in the chest leads. NONE of these changes are definitive. ALL of them are subtle — but taken together, this makes 6 out of 12 leads that are not as expected for a simple complete RBBB in a patient “old enough” to have something (74 years old) — and seen on this ECG that is of extremely poor resolution. BOTTOM LINE: Clinical correlation is essential for knowing how to interpret the above ECG findings on this tracing. IF the reason this ECG was done is new chest pain — then the onus is on us to determine IF an acute event might be in progress.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Machine interpretation
I would like your opinion on medicolegal aspect when ECG interpretation wrongly says ACUTE MI. Many thanks!
Mario Parrinello
A Common But Tough Problem
The ECG machine interpretations are notorious for being inaccurate and they certainly create a problem when they suggest a finding that actually does not appear in the tracing. A clinical history is vitally important in the interpretation of any 12-lead ECG, and rhythm strips too! I pity the cardiologist that has to overread ECG after ECG, often days after they were done, and with no idea why the ECG was ordered in the first place. As complex and fascinating as it is, the ECG remains an adjunct to the human brain.
I would certainly want to know if the patient had chest pain at any point and also if the RBBB was present on previous ECGs. If he had chest pain and there was no prior history of RBBB, then the possibility of a very proximal LAD occlusion must be entertained.
In addressing the medicolegal aspect, the treating physician will have more support from the history, the physical exam, biomarkers and his/her own (hopefully) educated evaluation of the ECG tracing to support a reasonable opinion regarding the diagnosis. Those factors will be a lot more defensible in court than simply relying on a machine interpretation that is KNOWN to be unreliable.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd