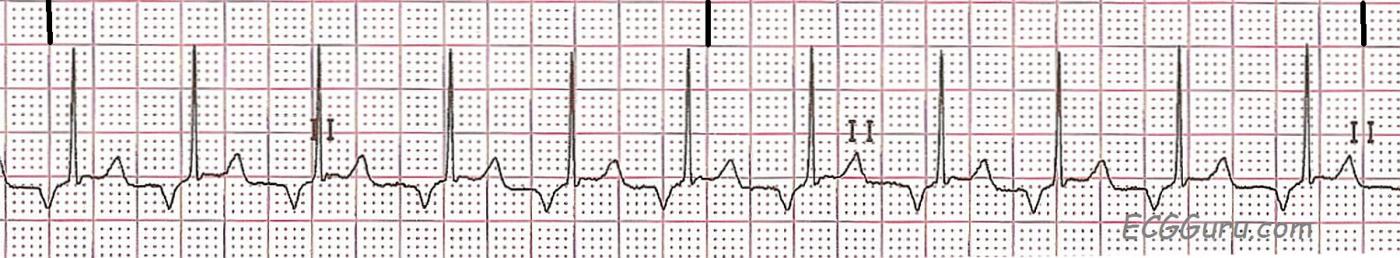
This Lead II rhythm strip shows a regular rhythm with narrow QRS complexes and retrograde P waves. The strip was taken from a nine-year-old girl. The rate is about 110 per minute and the PR interval is .12 seconds (120 ms).
When retrograde conduction is seen in the atria, it is often assumed that the rhythm is originating in the junction. When a junctional pacemaker is initiating the rhythm, the atria and ventricles are depolarized almost simultaneously. This can produce a P wave in front of the QRS with a short PR interval, during the QRS, or after the QRS. Sometimes, in junctional rhythm, a block prevents the impulse from entering the atria, producing NO P wave. Junctional rhythms are usually slow "escape" rhythms, but can be accelerated or tachycardic.
The fact that this rate is 110 / minute and the PR interval is normal at .12 seconds, we should consider that this rhythm could also be from an ectopic pacemaker low in the atria. From this low starting point, the impulse will travel backward, in a "retrograde" fashion, through the atria, producing a negatively-deflected P wave in Lead II.
We do not have clinical data on this patient, and so do not know what possible causes of arrhythmia might be present, and what the expected rate should be in this situation.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Retrograde P Waves - Confusing for Many
Dawn…
Retrograde P waves confuse so many newcomers to ECG interpretation. Somewhere along the line, they fall prey to several widespread misconceptions about retrograde P waves:
1. Retrograde P waves come from impulses originating in the junction or the ventricles.
As you pointed out, that is not entirely correct. An atrial impulse originating in the lower right atrium can also result in retrograde P waves.
2. All retrograde P waves are inverted – that’s how you tell they are retrograde.
Untrue. Not all retrograde P waves are inverted and not all inverted P waves are retrograde. For a P wave to be retrograde, it must be inverted in the inferior leads (II, III and aVF). Sinus P waves are sometimes inverted in Leads III and aVL and certainly in V1. Any P wave whose axis is more negative than +30° will be inverted in Lead III and any P wave whose axis is more positive than +60° will be inverted in Lead aVL.
3. Retrograde P waves always follow the QRS.
Again, untrue as you pointed out. Retrograde P waves can occur in front of, during or after the QRS complex. A retrograde P wave that originates in a focus in the lower right atrium can have a normal, prolonged or short PR interval (though usually not shorter than 0.10 seconds). A retrograde P wave due to a junctional ectopic beat may precede the QRS but generally not by more than 0.07 or 0.08 seconds. Retrograde P waves caused by ventricular ectopic beats that conduct retrogradely through the AV node NEVER precede the QRS complex.
Because the vector of a retrograde P wave has a superior direction, it will be more or less perpendicular to Lead I; therefore, retrograde P waves are often isoelectric in Lead I (or nearly so) and can be difficult to see in that lead. When you CAN see a retrograde P wave in Lead I, it will be upright. They will also be upright in leads aVR, aVL and the right-sided precordial leads (though V3 and V4 can be somewhat variable). Although retrograde P waves travel superiorly (unlike sinus P waves) they also travel to the left (just like sinus P waves). Therefore, since Lead I is a left-sided lead, if you can see a retrograde P wave in it at all, it will be upright due to the leftward vector.
The left-sided precordial leads (V5 – V6) can sometimes show the retrograde P waves as upright and sometimes inverted. Now why is that? The electrodes for these leads are often placed below the electrical center of the heart, either because of the patient’s body shape or (more likely) because the electrodes were not positioned correctly on the chest wall. If V5 and V6 are located BELOW the electrical center, retrograde P waves will usually be inverted in those leads since they will be acting like inferior leads (just like Leads II, III and aVF); if located above the electrical center, they are typically upright.
When the electrode for V6 is positioned correctly, V6 will usually reflect whatever Lead I is doing.
Hope this helps…
Jerry W. Jones MD FACEP FAAEM
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
Thanks, Dr. Jones
What a great, succinct, comment on retrograde P waves. Very helpful! The "ECG Basics" section of the ECG Guru shows only one- or two-lead ECG strips, because so many of our visitors are just beginning their training, or working in a setting where 12-Lead interpretation is not done. They don't yet know how to assess ECGs using multiple leads, and do not know about axis determination. I hope your comments will help the teachers of beginners understand the topic better, and not accidentally teach "facts" that have to be "un-taught" later. I also hope beginners will be intrigued to find out more about the subject, as ECG is a tool that is as useful as the interpreter's skills. While it is possible to get by with elementary understanding of the basic rhythms, it is so much better (and lots more fun) to learn and do more with ECG.
Dawn Altman, Admin