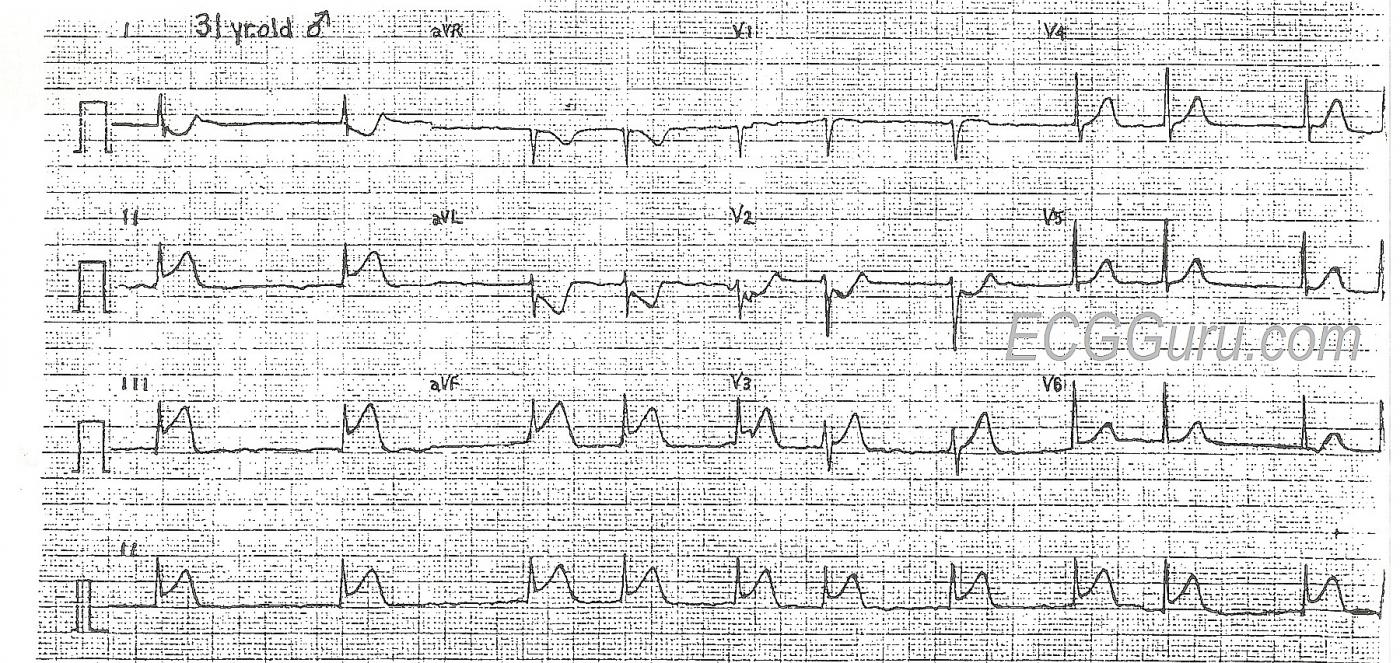
This 31-year-old man presented to the Emergency Dept. complaining of chest pain, shortness of breath, and nausea. His heart rate on admission was 120 - 130 bpm and irregular, and the monitor showed atrial fibrillation. His rate slowed with the administration of diltiazem. His 12-lead ECG shows the classic ST elevation of inferior wall M.I. in Leads II, III, and aVF. This patient also had JVD, bibasilar rales, orthopnea, and exertional dyspnea, signs of CHF. He had no history of acute M.I., CHF, or atrial fibrillation. He offered no history of drug use or medications.
This ECG is very useful for the basic student, in that the ST elevations are readily seen, and the atrial fib is definitely irregularly-irregular. For the more advanced student, the ST depression in V2 indicates posterior wall injury, while the flat ST segment in V1 indicates a possible right ventricular M.I. While the posterior wall is trying to depress the ST segment, the right ventricle is trying to elevate it, resulting in flattening. Also, Lead III has a greater STE than Lead II, which has been shown to be a reliable indicator of RV infarction. This should be confirmed with a V4 right, or all chest leads done on the right side. Right ventricular injury has been shown to increase mortality, and it also requires different management of hemodynamics.
It is unusual for a 31-year-old to experience acute M.I. That makes it important to rule out other causes of ST elevation and chest pain. Benign early repolarization and pericarditis should be considered. Some of the ECG signs that FAVOR the diagnosis of STEMI are: 1) ST segments are straight, rather than curved downward like a smile. 2) ST elevations are seen in related leads - leads oriented over the inferior wall and right ventricle (II, III, aVF, V1). 3) Reciprocal ST depressions are seen in leads known to be reciprocal to the inferior leads (I, aVL) and leads reciprocal to the "upper" inferior wall, or posterior wall. 4) There is an acute dysrhythmia (atrial fib). Atrial fibrillation is a fairly common complication of acute M.I., and also leads to increased mortality, especially when associated with CHF.
This ECG can start a very instructive discussion on the relationship between acute M.I., acute CHF, and new-onset atrial fibrillation. That could be an entire class by itself!
This patient was transferred to a nearby interventional cath lab, and his outcome is unknown.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Acute RCA Occlusion with AFib and perhaps Retrograde Wenckebach?
Ken Grauer, MD www.kg-ekgpress.com [email protected]
Possible AV nodal rhythm with Wenckebach block
Just seeing this now, but to continue with Ken’s speculation about the rhythm – is it possible that this is AF but with an accelerated AV nodal rhythm/nodal tachycardia (discharge rate approx. 100/min) with 2nd degree AV block? I think it is possible to interpret the ECG as showing 3:1 block at the start, then a mixture of 3:2 Wenckebach and 2:1 block. This is pure speculation with no evidence to support it but the timing of the QRS complexes does not seem completely random.
Dave R