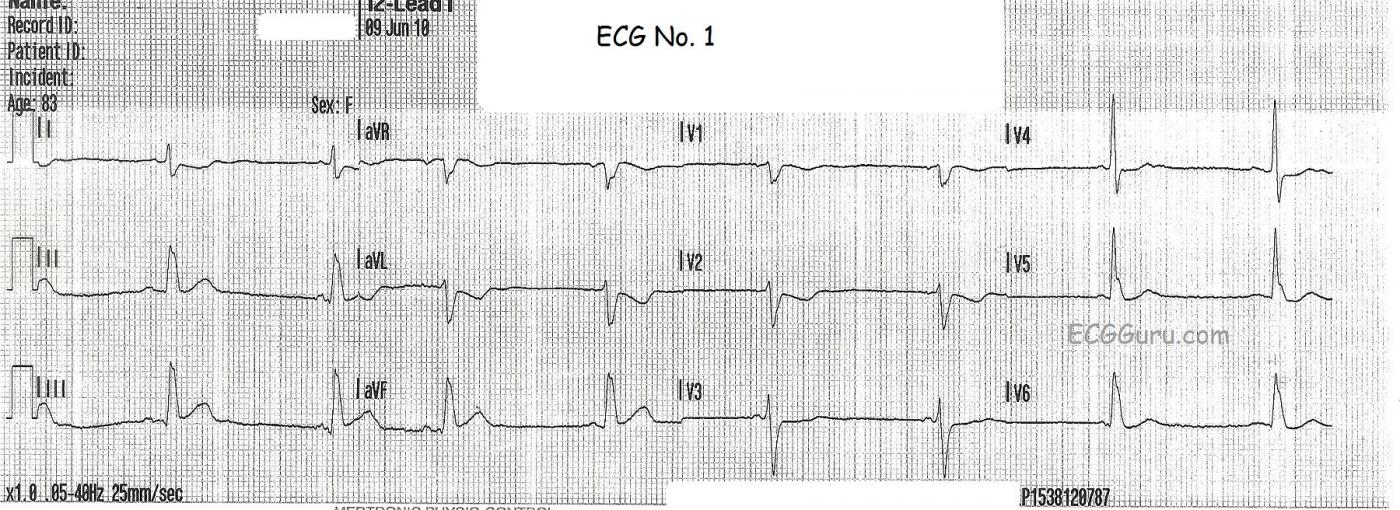
Continuing with our theme of using series of ECGs for teaching, we present the case of an 83-year-old woman with weakness, chest pain, and near-syncope. The first ECG, taken by paramedics at her home, shows a sinus rhythm with a slightly wide QRS complex. At this point, it is unclear whether this represents left bundle branch block or a non-specific interventricular conduction delay. There is the most subtle ST elevation in Leads III and aVF. In LBBB without acute M.I., we would expect the ST segments to be discordant, or opposite, the QRS complexes. Even more informative is the reciprocal ST depression in Leads I and aVL (and a little in V2). This can be a sign of inferior wall injury that shows up earlier than ST elevation in the inferior leads.
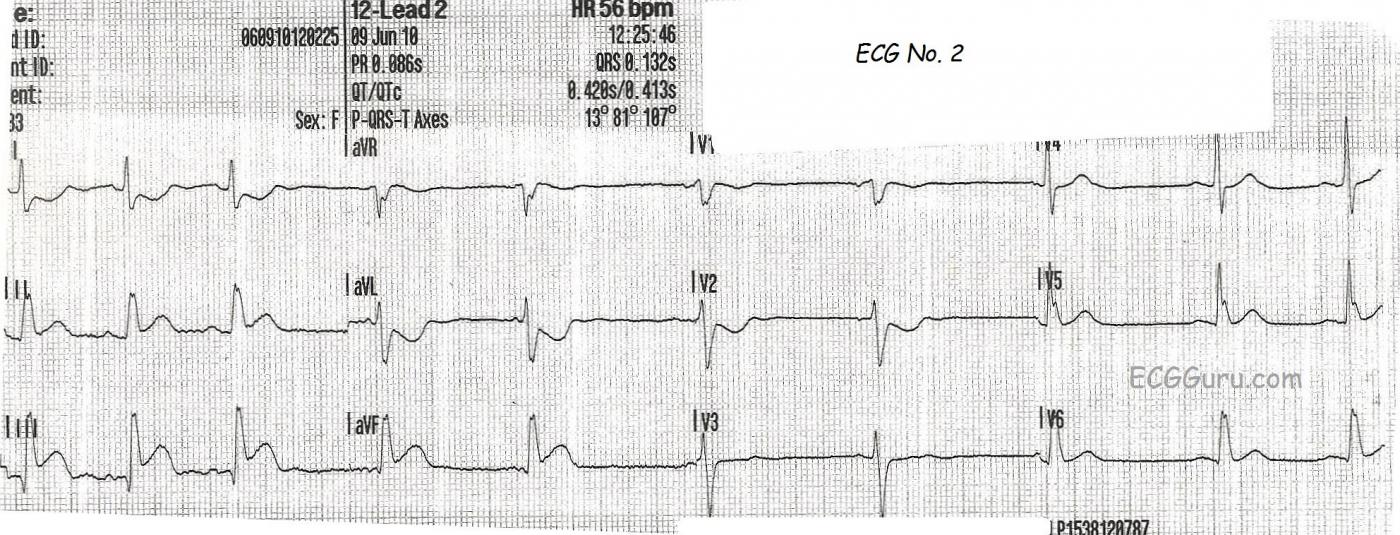
ECG number 2 was taken during transport to the hospital. The chest pain continues, and now the ST elevation in the inferior leads is pronounced, and the reciprocal depression in I, aVL, and V2 has also become much more obvious. V1 would also normally show this depression - a sign of the injury traveling up the back of the inferior wall (posterior). But if the right ventricle is injured, V1 will have ST elevation. V1 in this case is probably reflecting the depression from the posterior wall AND the elevation from the right ventricle. The ST elevation is now prominent enough that the paramedics notified the hospital of a "STEMI Alert". The QRS remains widened at .13 sec., but the ST elevations and depressions are not opposite the QRS direction, which would be typical for LBBB without an M.I. Therefore, even if LBBB is present, these ST elevations and depressions would be considered a sign of STEMI. The rate is slowing in this ECG.
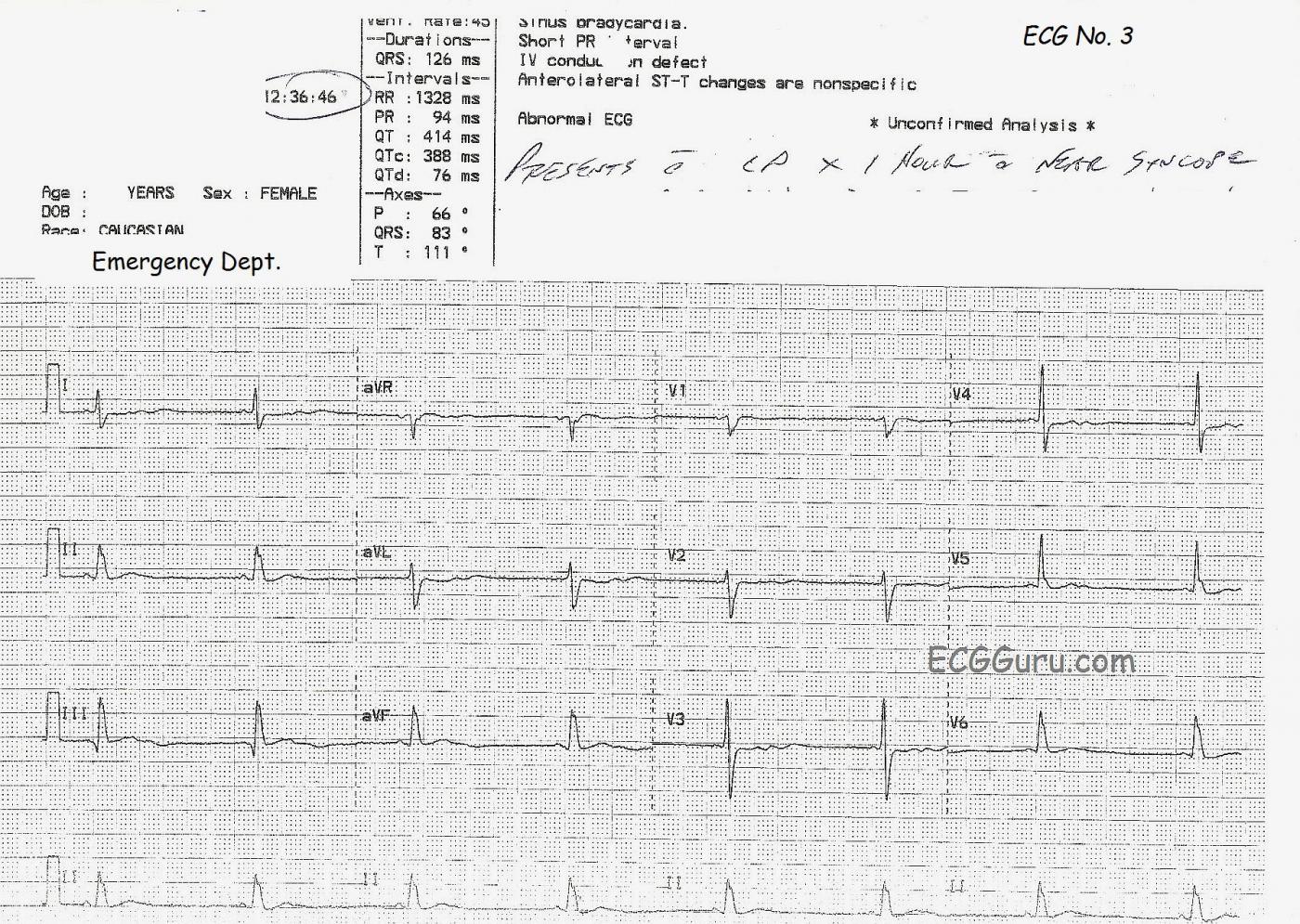
ECG number 3 was taken in the Emergency Department. The patient's symptoms continued. The bradycardia is still present, as is the QRS widening. Now, something new has shown up: prominent U waves in the precordial leads. There appears to be T-U fusion. We do not know the patient's medications or lab results, so the most likely cause for the prominent U waves is the bradycardia. She does not have other ECG signs of hypokalemia, which is one of the many causes of U waves.
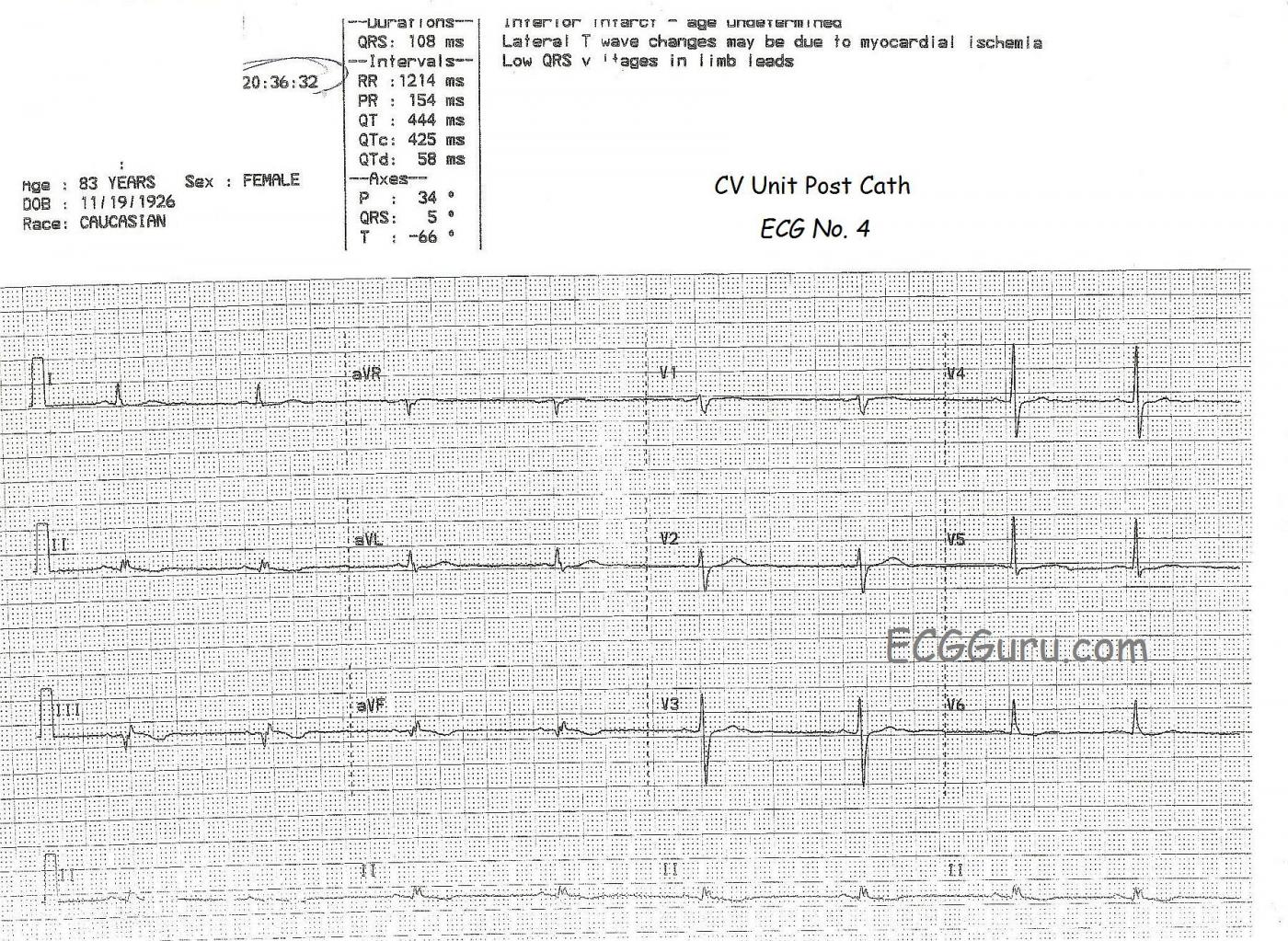
The patient was taken to the cath lab for angioplasty. In the cath lab, her right coronary artery was found to have several serious lesions, one of which was almost 100%. These lesions were stented. Often, when lesions are not completely occluding the artery, ST elevation can come and go. Arteries dilate and constrict, allowing more or less blood to flow past the partial occlusion. Changing arterial diameter, fluctuant thrombi, or increased/decreased myocardial oxygen demand can cause the ST segments to rise and fall. Changes in the nature of the chest pain can occur as well.
This ECG shows a continuing bradycardia (which may be affected by her medications), but her QRS has narrowed to .108 seconds (108 ms). Her inferior leads show a very slight coving upward of the ST segment, with T wave inversion, signs of evolution of the M.I. Unfortunately, pathological Q waves have formed in Leads III and aVF, which probably reflect permanent damage to the inferior wall. Followup ventriculograms or echocardiograms can establish LV function as time goes on. The good news is that the patient received good relief of her symptoms from the angioplasty procedure, and she did well to hospital discharge. We do not know about her condition post discharge.
To see images from this patient's RCA angioplasty, click HERE.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.