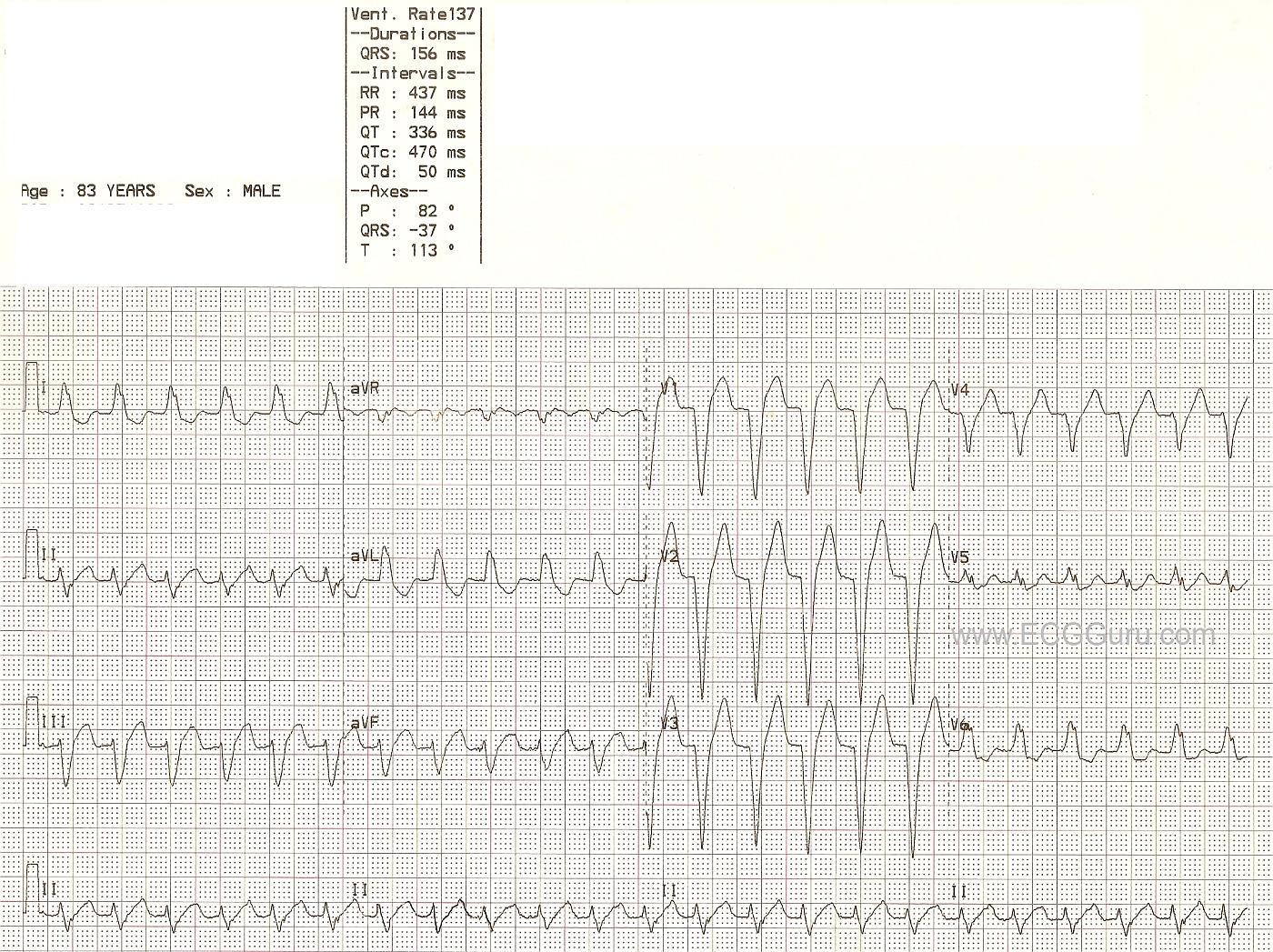
Today, we are revisiting an ECG from the archives, with a NEW comment from Dr Ken Grauer. This ECG is worth a second look because it is a very good example of the left bundle branch block pattern. It's also a good ECG to use when discussing treatment of wide-QRS tachycardias.
This ECG demonstrates a wide complex tachycardia with classic signs of LBBB: wide QRS, QRS negative in V1 and positive in V6 and Lead I, and supraventricular rhythm. P waves are difficult, if not impossible, to discern for sure. The machine does give a P wave axis and PR interval. When evaluating a wide complex tachycardia, the patient's hemodynamic stability will initially determine treatment. All WCTs should be treated as V TACH until proven otherwise. The presence of a typical LBBB pattern makes LBBB very likely, but is not a sure thing. This patient was confirmed to have LBBB when the rate slowed, the P waves became visible, and the QRS complexes did not change.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Regular WCT with LBBB Morphology
This ECG provides an excellent opportunity for review of the decision-making process for assessing the Regular WCT ( = Wide-Complex Tachycardia) when sinus P waves are not evident. The 1st Step (as implied by Dawn) — is to assess the patient for hemodynamic stability. If the patient is hemodynamically unstable — then diagnosis of the specific arrhythmia takes far less priority than immediate electrical cardioversion. However, IF the patient is hemodynamically stable (as we assume is the case here) — then there IS at least some time for arrhythmia assessment. Initial rhythm assessment of the hemodynamically stable patient can (and should) be fast — taking no more than a few seconds.
There are 5 basic parameters to assess. These are easily recalled by the saying, “Watch your Ps, Qs and the 3 Rs”. There are no P waves. The QRS is obviously wide. The rhythm is regular — the rate is ~ 135/minute — and since there are no P waves, there is no relationship between atrial and ventricular activity. Thus, we have described a regular WCT rhythm without P waves.
As Dawn mentioned — VT should always be assumed for any regular WCT rhythm in which atrial activity is absent. That said, even if the rhythm is VT — since the patient is stable, it is not unreasonable to consider initial trial of medical therapy.
That said, in this case — I suspect the rhythm is not VT, but some type of SVT ( = SupraVentricular Tachcardia). That’s because QRS morphology is absolutely typical for LBBB (Left Bundle Branch Block). Not only is there a completely monophasic R wave in the key lateral leads (I, aVL, V6) — but the QRS complex is all negative with very steep downslope to the S waves in leads V1,V2,V3. So while we cannot with certainty rule out the possibility of VT — my hunch is that the rhythm is an SVT.
The principal differential diagnosis of a regular SVT rhythm without sinus P waves is: i) Sinus Tachycardia (in which P waves are hiding within the previous T wave); ii) Atrial Flutter (with 2:1 AV conduction); iii) Atrial Tachycardia; or iv) a Reentry SVT Rhythm (such as AVNRT). Unfortunately, it is impossible to distinguish with certainty between these entities. That said — my hunch is that the rhythm is either sinus tachycardia or a reentry SVT. Review of previous ECG would be invaluable for seeing if QRS widening due to LBBB has been present. If so, this would rule out VT. Review of recent telemetry monitoring could be equally insightful. Sinus tachycardia usually gradually increases the rate — so P waves might be evident on earlier strips when the rate was slower. In this case, for this rhythm to be sinus tachycardia — the PR interval would probably have to be long (since we don’t see even a hint of P wave in either leads II or V1 during the tachycardia). Similarly, with atrial tachycardia — I’d expect to see some hint of atrial activity during the WCT rhythm. The ventricular rate is a little slow for atrial flutter (which usually manifests a ventricular rate closer to 150/minute) — and 2:1 flutter waves are usually evident when looked for in at least some leads. So my hunch as the two most likely possibilities are either sinus tachycardia with preexisting 1st degree AV block or a reentry SVT. IF the patient is stable, trial of a vagal maneuver and/or “chemical valsalva” with Adenosine would be my initial approach, given my strong suspicion that the rhythm is an SVT. Adenosine would slow the rhythm and enable definitive diagnosis if this is sinus tachycardia. If instead this is a reentry SVT — then Adenosine will most likely successfully convert the rhythm. Of course, if at any time during the process the patient shows sign of decompensating — immediate cardioversion is then in order.
-------------------------
Ken Grauer, MD www.kg-ekgpress.com [email protected]