The Patient: A 78-year-old woman called emergency responders because she had palpitations. She was alert and oriented. Her BP was reported as being “stable”. We do not have information about her past medical history. We will update this post if we receive information about her outcome.
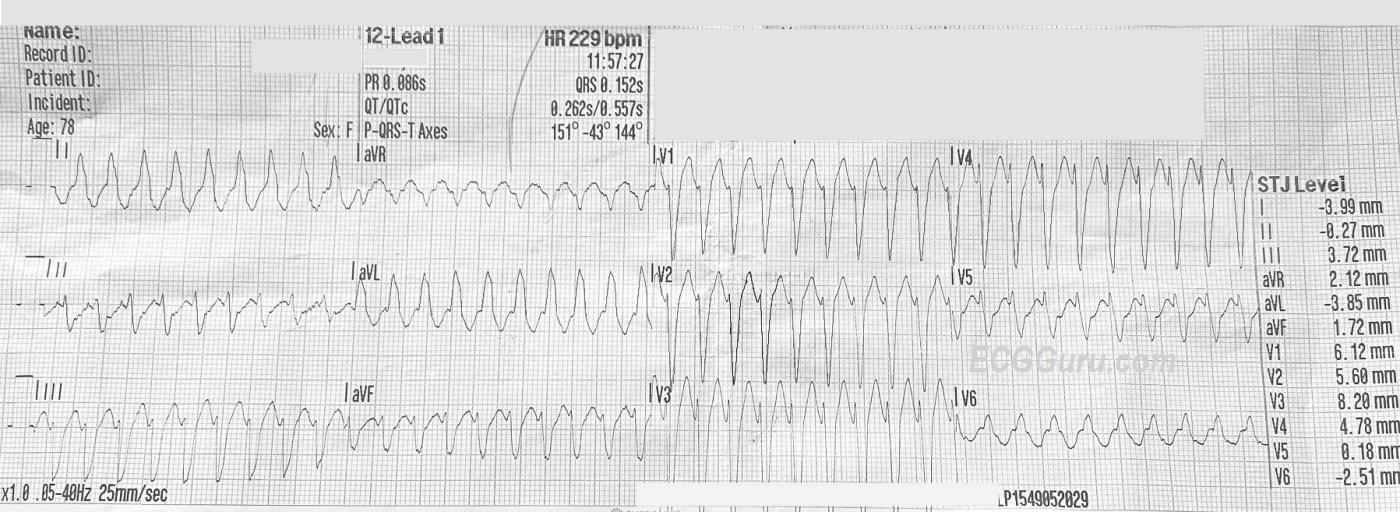
ECG Number 1, 11:57 a.m.: There is a wide-complex tachycardia at a rate of about 230 bpm. The QRS is .15 seconds (150 ms). The QRS frontal plane axis is leftward. P waves are not readily seen, but the computer gives a P axis and PRI. The PRI given is taken from Lead II, which, along with V5, does have P waves. In the other leads, the P waves are buried in preceding T waves. This photo shows an ECG that is not lying flat, so it is difficult to line up the complexes. Normally, it helps to look at the leads above or below to determine where waves begin and end, as all three channels are run simultaneously. The QRS complexes have a “typical” left bundle branch block morphology, with an rS complex in V1 and a monophasic R wave in Leads I and V6. The T waves are “discordant”, they are in the opposite direction from the QRS complexes, which is typical of LBBB.
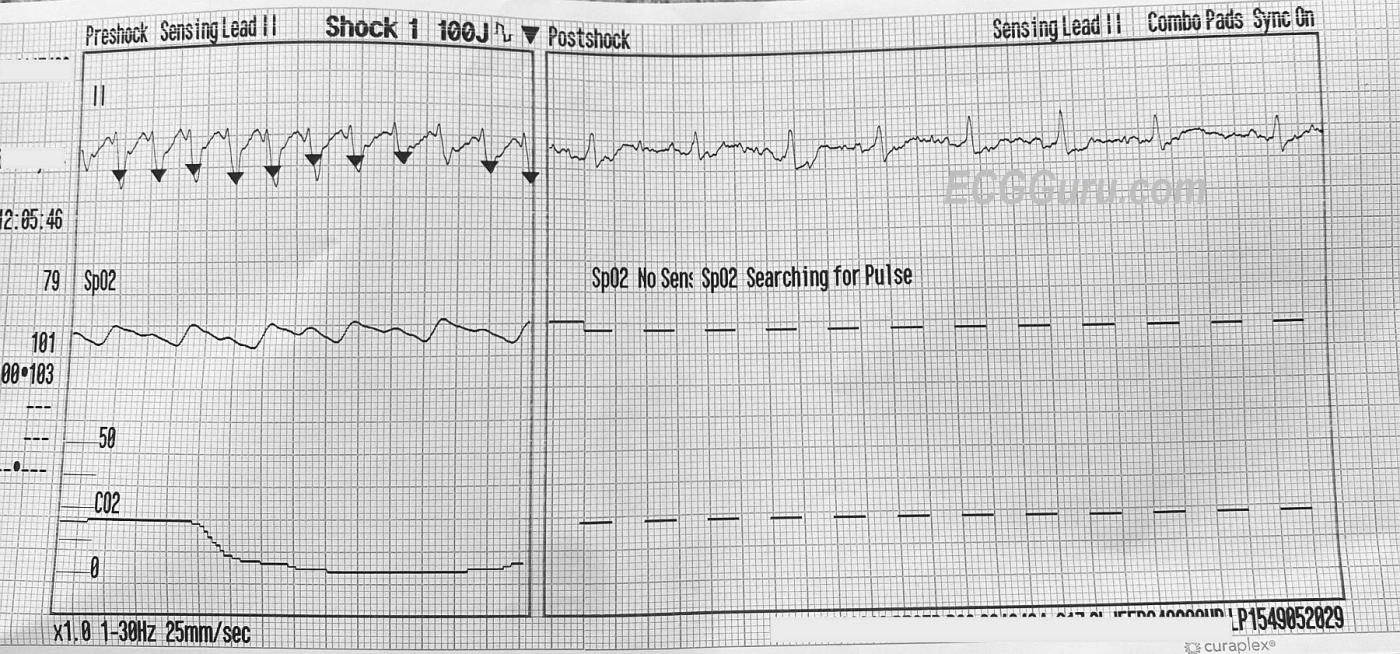
ECG Number 2, 12:05 p.m.: This is a rhythm strip recording a synchronized shock at 100 joules, resulting in conversion of the WCT to a narrow complex, irregular rhythm. It appears that there is a P wave before every narrow QRS, but artifact prevents proper evaluation.
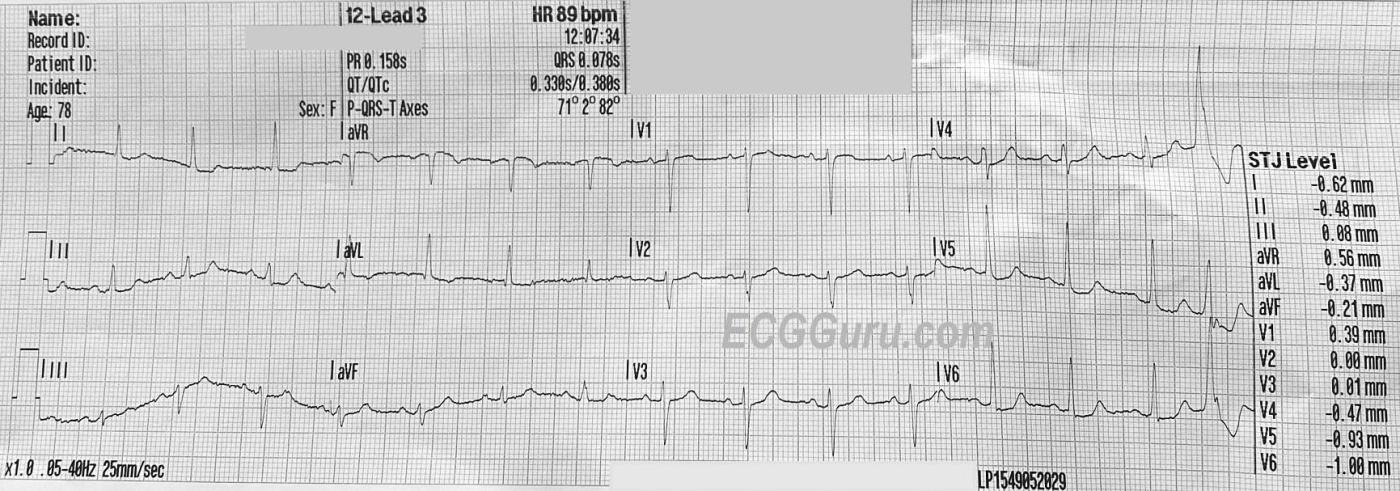
ECG Number 3, 12:07 p.m.: The post-cardioversion rhythm has settled into a sinus rhythm at about 90 bpm. There is a PVC near the end of this tracing. Notice that the PVC does not have the same appearance as the previous WCT, indicating that it came from a different focus. There are no obvious signs of STEMI, and the ST segments are mostly normal, with a tiny amount of elevation in V1 and ST depression in V5 and V6, if you look very closely. Remember, this is moments after cardioversion.
Discussion: Wide-complex tachycardia can present a diagnostic dilemma. Even experienced clinicians have difficulty determining whether a WCT is ventricular tachycardia or aberrantly-conducted supraventricular tachycardia (SVT-A). Complicating the matter is the fact that some ventricular tachycardias are relatively benign, and some are quite life-threatening. Also, there are many different dysrhythmias that fall into the category of “SVT”. Add “really wide WTC”, which is actually the effect of sepsis or electrolyte abnormality like hyperkalemia, and we do have a lot to think about.
Most EMS agencies in the United States have a WCT protocol which essentially is a safe approach to both VT and SVT-A. In the short time available to an emergency responder, it may be better not to spend the time trying to decipher the difference while the patient possibly deteriorates. These protocols generally allow for Amiodarone for “stable” patients, and electrical cardioversion for patients with low blood pressure and other signs of deteriorating perfusion status. Both VT and SVT-A respond well to electrical cardioversion.
This set of ECGs is very interesting. On first glance, I thought the WCT looked like VT from the right ventricle. On very close inspection, P waves are visible in Lead II, as mentioned above. They are associated with the QRSs (no AV dissociation). The pattern fits LBBB, favoring a diagnosis of aberrant SVT. It is common for a patient without bundle branch block to develop a BBB pattern when the rate accelerates. This doesn’t represent an actual “block”, but rather the impulse has arrived early and found the left bundle branch still refractory, while the right bundle branch has completely repolarized. The LBBB pattern disappeared as soon as the rhythm converted to NSR. There are other signs of SVT-A, such as a rapid onset of the QRS (measuring from the onset of the r wave in V1 to the nadir of the S wave, there is less than 100 msec., or 2.5 small blocks.) If you are an instructor or a clinician who is past the “beginner” stage of ECG interpretation, learn as much as you can about the various types of WCT and their treatments. We highly recommend a new workbook, written by Dr. Jerry Jones, in his very readable style. Getting Acquainted With Wide Complex Tachardias, A Workbook For the Electrocardiographically Confused. Available at Barnes & Noble and Amazon. It is not for the beginner, but is invaluable reading for the intermediate or advanced level practitioner. We also recommend Dr. Ken Grauer’s blog and YouTube Video blogs for a wealth of information on this topic. One especially helpful post is ECG Blog #42: What Criteria? VT vs. aberrancy? Dr. Grauer is the Contributing Expert for this website. Dr. Jones is a frequent contributor, and has a very informative blog on LinkedIn. Both have a unique ability to explain difficult topics like this one so that they are very understandable.
Our thanks to Travis Britt for donating this interesting case.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Regular WCT in a 78yo Woman — AVNRT?
Important case by Dawn — that illustrates a number of KEY concepts regarding evaluation and management of a regular WCT ( = Wide-Complex Tachycardia).
As per Dawn — the history is that of a 78-year old woman who called EMS for palpitations — but who otherwise appeared to be hemodynamically stable. No information regarding her previous health status.
The “good news” — is that this patient was hemodynamically stable with today’s initial ECG. The “other news” — is that given her age, our “threshold” to consider emergency cardioversion will be immediately lowered.
For clarity — I’ve put ECG #1 together with ECG #3, with a few added labels. I interpreted ECG #1 as showing a regular WCT at ~225/minute, without clear sign of P waves. To EMPHASIZE — identifying sinus P waves in a rhythm this fast is difficult, because of how short R-R intervals are. But I thought the PR interval would be too short if the upright deflection I’ve labeled with a RED line were to be a sinus P wave. In my experience — you’ll virtually never see P waves in lead V5 but not in leads V1, III, aVF — so I do not think there are sinus P waves, but instead just prominent T waves that simulate P waves because the rate is so fast. (NOTE: Against the RED lines being P waves is the reality that sinus tachycardia will not attain a rate of 225/minute in a 78 year woman …).
Instead — I suspected in my initial review of ECG #1 that the BLUE lines in ECG #1 represented retrograde P waves. I fully acknowledge it is impossible to prove this — but I believe the course of events in today’s case IS consistent with my assumption of retrograde P waves with a short RP’ interval in this patient with AVNRT.
As per Dawn — the computerized interpretation suggested a “normal” PR interval in ECG #1. That said — my 1st PEARL is to IGNORE the computer interpretation for ANY complex arrhythmia, because there are just too many false positives and false negatives for computerized ECG rhythm interpretation. In my opinion (based on 40+ years of careful observation) — there will NEVER be a sufficiently accurate computer ECG program for complex cardiac arrhythmias. Instead — the responsibility for the interpretation of complex arrhythmias lies with us! I say this with full appreciation and acknowledgment of the wonderful work that Drs. Stephen Smith and Pendell Meyers are accomplishing for attaining highly accurate computerized interpretations in the Queen Of Hearts application for identification of acute OMI ( = acute coronary occlusion MIs). That said — accurate computerized interpretation of complex arrhythmias is a completely other story (in my opinion).
I completely agree with Dawn that QRS morphology in ECG #1 is perfectly consistent with LBBB conduction. Not only are monophasic all upright R waves present in lateral leads I,aVL,V6 — and a predominantly negative QRS complex in right-sided lead V1 — but predominant negativity of the QRS extends to lead V5 — and the SLOPE of the downslope of the S waves in V1-thru-V4 is very steep, all consistent with supraventricular LBBB conduction.
BOTTOM LINE: Nothing is 100% — but given such typical QRS morphology for LBBB conduction AND what I perceive as 1:1 retrograde (V:A) conduction — I thought the rhythm diagnosis of ECG #1 most likely to be AVNRT with QRS widening manifesting LBBB conduction due EITHER to preexisting LBBB — OR — to LBBB aberration.
What to do depends. Again — a rate of 225/minute in a 78 year old person is not something I would want to leave for a long time. As to whether I would try Adenosine or Amiodarone before cardioverting — would depend. Either action might be reasonable — and “Ya just gotta be there” to know what you feel would be best “at the bedside”, given the circumstances.
NOTE: The reason I would consider Adenosine — is that this drug in my opinion, would have highest chance of prompt success in converting this rhythm that I suspect is AVNRT with LBBB conduction. I realize and accept that others may disagree — and I don’t think anyone can know with certainty what the rhythm is in ECG #1 from this single tracing.
The patient was electrically cardioverted — and sinus rhythm was restored. Note that the PR interval is clearly longer in the post-conversion tracing than in ECG #1 (GREEN lines). Note also that with sinus rhythm — definite sinus P waves are also seen in leads III,aVF and V1. While true that the PR interval does shorten with tachycardia — it does not usually shorten as much as it would have to if the RED arrows in lead II of ECG #1 were P waves.
As per Dawn — a PVC is seen at the end of the post-conversion tracing — with a different QRS morphology than for the WCT (ie, the QRS is all positive in leads V4,5,6 for this PVC — whereas there should be predominant negativity in leads V4,V5 if there was LBBB conduction).
NOTE: The fact that with sinus rhythm in the post-conversion tracing the QRS is narrow — tells us that the reason for LBBB conduction during the tachycardia was not “preexisting BBB” — but rather rate-related LBBB aberration.
FINAL THOUGHT: In the post-conversion ECG — there is nonspecific ST segment flattening in multiple leads, with some ST depression in a number of leads — and with ST elevation in lead aVR. This is not a “normal” ECG — and in a 78 year old woman, it may represent underlying coronary disease. While true that it is common to see ST-T wave abnormalities following a sustained tachycardia — it should be kept in mind that further evaluation of this 78 year old patient will be important for determing longterm management (ie, Potential need to consider a rate-slowing medication to prevent SVT recurrence and/or possible need to evaluate for underlying coronary disease).
Ken Grauer, MD www.kg-ekgpress.com [email protected]