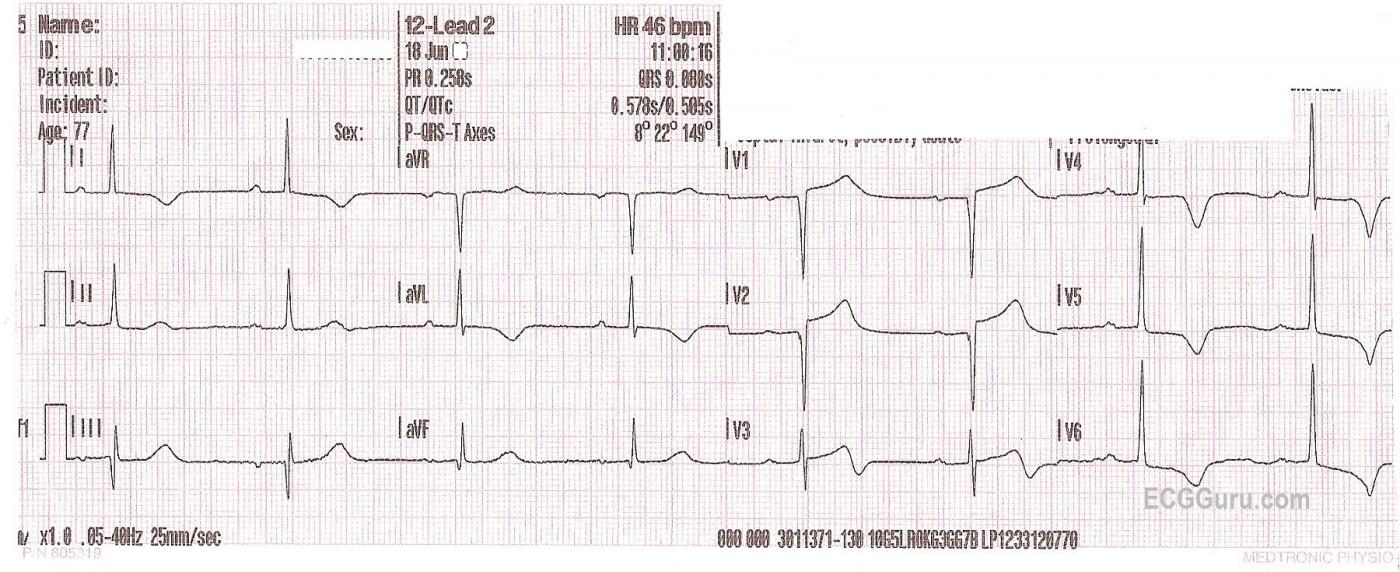
A 77-year-old man was brought to the Emergency Department with stroke symptoms. He had less than one hour since symptom onset. He presented with extreme weakness of his right side and slurred speech. He has a history of coronary artery disease and previous acute M.I. His BP was 188/80, P 46/min., and resp. 16/min. He denies chest pain, N&V, and shortness of breath. The E.D. physician called in the stroke team, and a diagnosis of CVA was made. What does his ECG show?
This ECG shows clear ST elevations in V1 and V2, with abnormally flat ST segments in nearly all leads. In addition, there are ischemic T wave inversions in Leads V3, V4, V5, I, and aVL. A diagnosis of anterio-lateral M.I. is made in addition to stroke.
Ischemic changes, like ST elevation and T wave inversions have been demonstrated frequently in patients with strokes. Stroke symptoms have also been recorded in patients who are having M.I.s. Ischemic stroke has been shown to be a complication of acute myocardial infarction. Hemorrhagic stroke can follow anticoagulation or thrombolysis. Also, acute M.I. has been shown to be a complication of stroke. Artery disease is a common denominator in both conditions.
Needless to say, this can be a very complex problem, and the patient with stroke symptoms requires a CT scan to rule out hemorrhage before the M.I. is treated with anticoagulants or thrombolytics.
References: MI After Stroke, The Heart.org; Incidence of Stroke After Acute M.I., Witt, et al ; Ischemic Stroke After Acute Myocardial Infarction, Mooe, et al.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Stroke and Recent, Acute or Infarct-about-to-Happen?
Highly interesting case by Dawn. I believe it was the Framingham studies that first showed ~ 2-5% of acute stroke patients had an acute MI at the time of their presentation.
Important findings from this ECG are: i) fairly marked bradycardia; ii) probable LVH (just shy on voltage) with “strain” and/or ischemia - with really deep, symmetric T wave inversion in the lateral precordial leads; iii) a QT that seems long (goes along with acute CVA); iv) Q waves in III,aVF of uncertain significance; v) a QS complex in V1,V2 of uncertain significance; vi) J-point ST elevation in V1-thru-V3 of uncertain significance; and vii) Suspected Wellens’ Syndrome ST-T wave in lead V3 vs reperfusion ST-T segment in this and the lateral precordial leads ...
I do not see definite evidence of acute STEMI on this tracing. That is NOT to say that there isn’t an acute infarct yet. Perhaps this patient did infarct (producing those anterior QS complexes and ST elevation) and what we see in V3-thru-V6 represents reperfusion? - or perhaps there is a tight proximal LAD that has not yet occluded? Troponin values and serial tracings may provide insight. Certainly not an easy management case given associated acute stroke ….
Ken Grauer, MD www.kg-ekgpress.com [email protected]