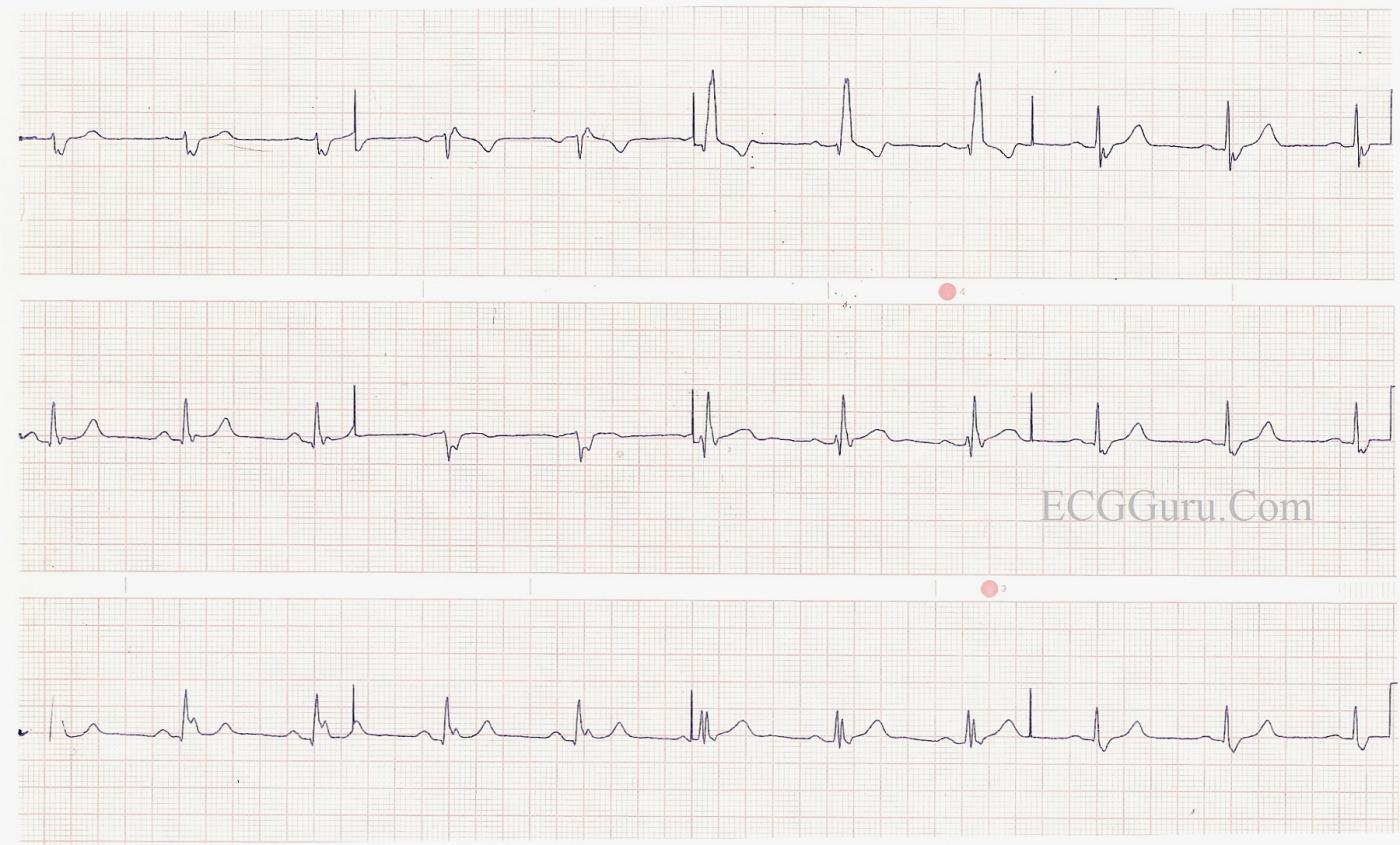
This is a good clear example of right bundle branch block with left posterior fascicular block. The RBBB is diagnosed by the following criteria: wide QRS (.12 sec), supraventricular rhythm (NSR), an rsR' pattern in V1, and wide little s waves in I and V6. The LPFB is inferred by the right axis deviation (Lead III QRS is a bit taller than Lead II and Leads I and aVL are negative), and the fact that there is no other obvious cause for right axis shift noted in this patient. This constitutes a BIFASCICULAR BLOCK. The ventricles are being depolarized by way of the anterior fascicle. In addition, there are slight ST elevations in many leads, with an upward coving in the anterior-septal leads (V1, V2, V3). Depending upon the patient's history and presentation, this could represent a recent M.I. or pending issues. The borderline first-degree AV block may be of concern in this patient, since first-degree AVB is associated with progression of bifascicular block to complete heart block. Reference: Ann Card Anaest, 2010 Jan-Apr;13(1):7-15. doi: 10.4103/0971-9784.58828
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
RBBB with True LPHB - and a LOT More to Comment On!
I will make a number of observations on this interesting example of RBBB posted by Dawn.
Ken Grauer, MD www.kg-ekgpress.com [email protected]