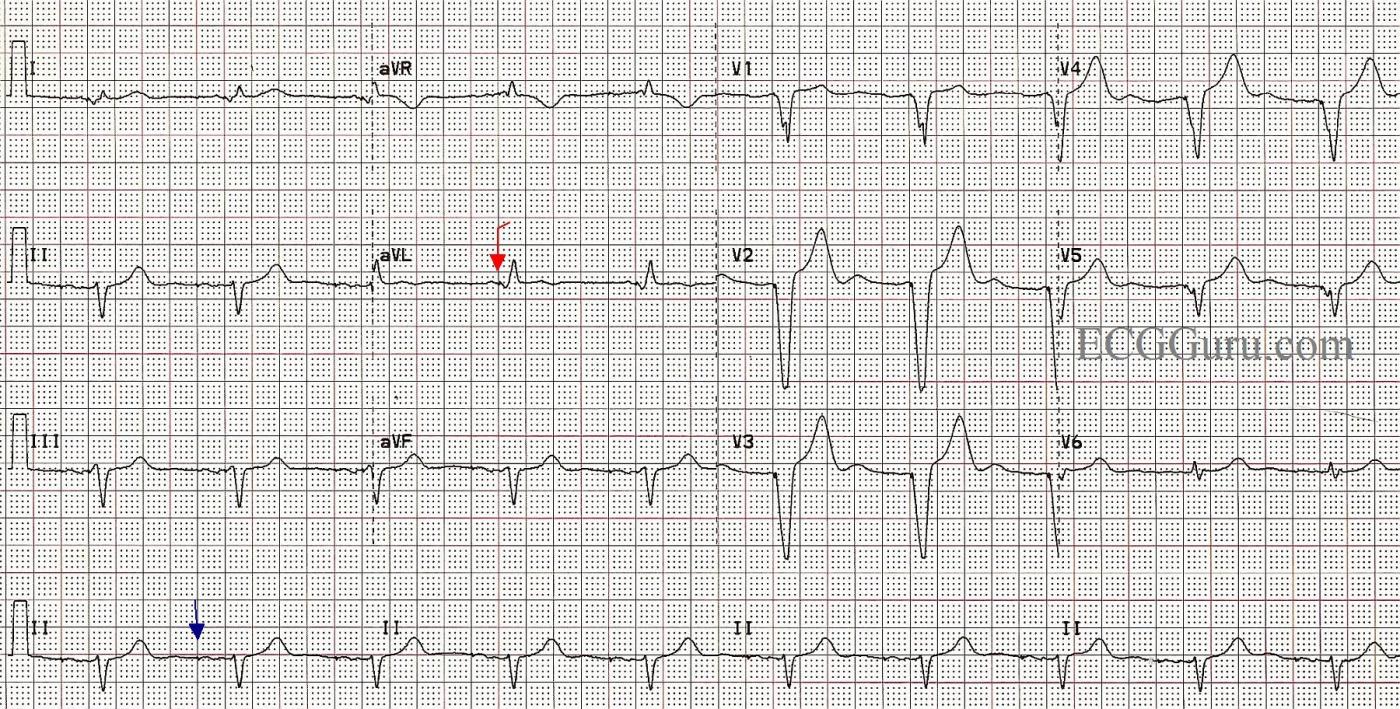
This ECG is taken from a woman who had suffered for several years with intractable intermittent atrial fibrillation. She had tolerated medications poorly, and several attempts at electric cardioversion had resulted in only temporary relief. Ultimately, she chose to undergo AV node ablation. In the electrophysiology lab, her AV node was destroyed, preventing the atrial fib impulses from penetrating into the ventricles. This resulted in a “man-made” complete AV block. A pacemaker was implanted in the EP lab. When she is in atrial fibrillation, the fibrillatory waves of the atria INHIBIT the atrial pacing electrode from firing, so she has no paced P waves at that time. The right ventricular pacing electrode functions without inhibition, and makes a wide QRS complex with a leftward axis deviation (normal for RV pacing).
In this ECG, we see the patient WITHOUT atrial fib, and the pacemaker is pacing the atria AND the ventricles, in a sequential fashion. The spikes are very hard to see, as this is a “bipolar” pacemaker, which makes much smaller spikes than a “unipolar” pacemaker. Some ECG machines will automatically enhance the spikes, but this one did not. We have marked a “sample” atrial spike in blue for you and one of the ventricular spikes in red. Each beat on this ECG actually has appropriately-timed atrial and ventricular stimuli (spikes), and the patient has optimized cardiac output provided by the “atrial kick”. A P wave occurring just before a QRS indicates that the ventricles are filling from the forceful contraction of the atria. This provides much better filling than when the atria are not beating or are fibrillating.
This is a good ECG to use to show your students how we can recognize a paced rhythm without being sure of the spikes. Of course, without other evidence (patient history and exam), we can’t know for sure that this is a paced rhythm, but the steady, normal rate, wide complexes, and left axis deviation are signs of RV pacing. Look for negatively-deflected QRS complexes in II, III, and aVF and positive QRSs in aVL and aVR.
When pacing only one ventricle, the impulse travels relatively slowly through the other ventricle, resulting in wide QRS complexes. This then results in SECONDARY ST-T WAVE CHANGES. Wherever the QRS is positive, you will normally see some ST depression and T wave inversion. In leads with negative QRS complexes, the opposite is true, and you will see ST elevation and upright T waves. This can make evaluation of ST segments for acute M.I. difficult.
All our content is FREE & COPYRIGHT FREE for non-commercial use
Please be courteous and leave any watermark or author attribution on content you reproduce.


Comments
Does this Patient have a Pacemaker?
There are a handful of situations for which I find myself looking at an ECG and asking, “Why am I unsure about what this tracing shows?”. Despite feeble attempts to reassure myself in the knowledge that as a teacher of electrocardiography and clinician who has interpreted literally thousands of difficult tracings — these perplexing encounters continue to occasionally pose problems for me. One of these situations is AFib (Atrial Fibrillation). While most of the time, the ECG diagnosis of AFib is obvious — sometimes this is not the case. The most notorious example of this phenomenon, is that ECG without prior comparison tracing — in which the rhythm looks almost regular; the ventricular response is controlled (ie, between 60-to-80/minute); P waves are absent; and the baseline is clean and devoid of those “telltale” undulations known as “fib waves”. More than once in such cases have I found myself asking whether I was looking at AFib or a slightly accelerated junctional response or simple sinus rhythm with extremely small P waves.
The other ECG encounter that occasionally has me wondering — is that patient with a pacemaker whose device leaves no more than the tiniest clue of mechanical stimulation. This tracing presented by Dawn provides an excellent example of this latter phenomenon. When I first looked at this ECG — I thought it represented some type of atypical LBBB. The clinical reality, is that we do not always know at the time we are asked to interpret a tracing whether or not the patient has a pacemaker. The patient’s medical record may not be available — and sometimes even the patient doesn’t know if they have a pacemaker … While pacemaker spikes are usually easy to see (at least in some leads …) — they are not at all obvious in any of the leads on this ECG. But, pacemaker spikes are present, and they are present in multiple leads:
BOTTOM LINE: The art of ECG interpretation is both fascinating and humbling. Failure to appreciate that a pacemaker is present in a tracing such as the one shown here — would be a fundamental oversight that could lead to a dramatically different clinical interpretation and management approach. Awareness of how this can happen, and the focus one must routinely devote to detect subtle pacemaker spikes will hopefully help to avoid this potential pitfall. It will also explain why even experienced clinicians sometimes ask, “Does this patient whose ECG I am trying to interpret have a pacemaker?”.
Ken Grauer, MD www.kg-ekgpress.com [email protected]
heart rate clue
In response to Ken's comments about the occasional genuine difficulty in being sure whether a rhythm is paced, the heart rate can provide a clue. Here the HR is EXACTLY 60/min throughout the recording. This doesn't prove anything but it certainly supports a suspicion of pacing. Of course, the converse is not true: A HR other than 60/min does not in any way exclude pacing.
Dave R
Re: "heart rate clue"
Certainly I agree with Drs. Grauer and Richley, but I think the key word in Dr. Richley's comment (which he conveniently capitalized) is "EXACTLY" and not the rate of 60/min. I'm not so concerned about the actual rate as the fact that the rhythm is perfectly - EXACTLY - regular. One of the first things I have my students do in my advanced ECG class is to use their calipers and try to find a sinus rhythm that remains exact for more than 6 or 8 beats. So, even if the rate were 68/min, 70/min or 75/min - the fact that it is EXACT throughout the tracing is an excellent hint that a pacemaker is present. I gave up thinking I could determine the presence of a pacemaker by the miniscule pacing spike a long time ago. I really think the pacemaker manufacturers have done healthcare providers a real disservice in not making the pacemaker artifacts more visible.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd
Small pacing spikes
In response to Dr Jones’s comments about the difficulty in identifying tiny pacemaker ‘spikes’ on ECGs, there are a number of factors that may contribute to this. One is the indiscriminate use of filters by the ECG machine user. Many people seem to have all the filters switched on as the default position in order to eliminate ‘noise’, but one effect of the low-pass filter can be to greatly attenuate the amplitude of the pacing spike. Secondly, nearly all pacing is bipolar rather than unipolar these days, which avoids inappropriate pectoral muscle stimulation but does mean that the pacing artefact will be small. Lastly, it is current practice (no pun intended) to pace at a much lower output than used to be the case, to prolong battery life. Many pacemakers repeatedly measure the pacing threshold and continually adjust their output themselves accordingly to pace at the lowest voltage that guarantees effective capture. Long gone are the days of standard pacing at 5 volts for 0.5 ms (which I remember)! Again, low output pacing has the effect of producing very small pacing artefacts. In order to get round this problem some ECG machines, by sampling at a very high rate, will detect the pacing stimulus and indicate its occurrence by producing an artificially big pacing spike. This clearly shows that pacing is taking place, but the artificial representation of the pacing impulse is of a fixed size which bears to relation to the size of the actual stimulus. This is useful for identifying pacing but it does mean that real variations in the size of the detected pacing stimulus that may indicate, for example, that the pacing lead has become dislodged, will not be displayed. For this reason, it may be diagnostically more useful to display pacing artefacts as they are detected even though the deflections on the ECG paper may be very small. This is quite a complex subject (on which I am no expert) but I do think that a combination of the over-use of ECG machine filters and advances in pacing technology is making it more difficult to detect pacing stimulation on the ECG.
Dave R
Addendum to my comment
Of course, an escape rhythm could be "exact" for the 10 seconds or so duration of an ECG and reentrant rhythms can be exact (though, obviously, much faster). So, as Dr. Grauer pointed out, knowing the circumstances surrounding the acquisition of the ECG is extremely helpful.
Jerry W. Jones MD FACEP FAAEM
https://www.medicusofhouston.com
Twitter: @jwjmd